Horizontal diffusion cells simulate the in vivo environment primarily through precise temperature regulation and hydrodynamic agitation. They utilize a water-bath jacket to maintain a stable temperature of 32±0.5 °C—replicating the surface temperature of human skin—and employ internal magnetic stirring to ensure fluid uniformity, mimicking the circulatory system's removal of drugs from tissue.
By stabilizing the thermal environment and maintaining constant fluid movement, these cells allow researchers to replicate the dynamic process of drug penetration across biological membranes under "sink conditions."
The Mechanics of Physiological Simulation
Mimicking Skin Surface Temperature
Horizontal diffusion cells are designed to replicate the specific thermal conditions of the skin's surface, rather than the body's core temperature.
To achieve this, the device employs a water-bath jacket that circulates warm water around the cell.
This system maintains the environment at 32±0.5 °C. This is critical because skin permeability is highly temperature-dependent, and 32°C accurately reflects the external temperature of human skin.
Simulating Blood Circulation
In a living organism, once a drug penetrates the skin, it is swept away by blood flow. This prevents the drug from accumulating at the absorption site.
Horizontal cells simulate this dynamic clearance through internal magnetic stirring.
The stirring mechanism keeps the receptor liquid—typically a phosphate buffer—uniformly mixed. This prevents high concentrations of the drug from building up directly beneath the membrane.
The Role of Biological Membranes
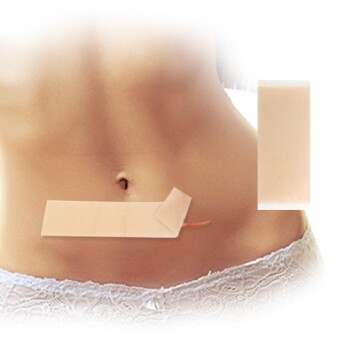
To complete the simulation, a biological barrier is placed between the donor and receptor compartments.
As noted in standard protocols, researchers often use excised rat skin or similar biological membranes in this position.
This setup mimics the actual physical barrier the drug must navigate to enter the circulatory system.
The Importance of "Sink Conditions"
Maintaining a Concentration Gradient
For a permeation experiment to be valid, it must maintain sink conditions.
This means the concentration of the drug in the receptor chamber (the "blood") must remain significantly lower than in the donor chamber (the "skin surface").
Why Uniformity Matters
Without the uniformity provided by magnetic stirring, the drug would pool near the membrane.
This pooling would artificially slow down the diffusion rate, leading to inaccurate data regarding how the drug will perform in a living patient.
Understanding the Trade-offs
Temperature Selection
While the primary standard for skin permeation is 32°C, confusion often arises regarding physiological temperature.
Some experimental protocols may attempt to use 37°C (core body temperature). However, for topical applications, 32°C is the most accurate reflection of the skin barrier's environment. Using 37°C may artificially increase permeation rates.
Model Limitations
While horizontal cells provide a robust simulation, they are an in vitro model.
They accurately simulate passive diffusion but may not fully capture active biological processes, such as metabolism within the skin or variations in blood flow rates due to vasoconstriction.
Making the Right Choice for Your Goal
When configuring your horizontal diffusion cell experiment, align your parameters with your specific research objective.
- If your primary focus is topical dermatological formulations: Ensure your water jacket is strictly calibrated to 32°C to reflect the skin surface environment accurately.
- If your primary focus is deep tissue or systemic absorption: Prioritize the magnetic stirring speed to rigorously maintain sink conditions, ensuring the receptor fluid never approaches saturation.
Success in skin permeation testing relies on the precise replication of the body's thermal and hydrodynamic barriers.
Summary Table:
| Feature | Physiological Component | Simulation Mechanism | Standard Parameter |
|---|---|---|---|
| Temperature | Human Skin Surface | Water-bath Jacket | 32±0.5 °C |
| Circulation | Blood Flow / Clearance | Magnetic Stirring | Constant RPM for Sink Conditions |
| Barrier | Stratum Corneum / Dermis | Excised Skin / Membrane | Biological or Synthetic |
| Medium | Extracellular Fluid | Receptor Liquid | Phosphate Buffer (pH 7.4) |
Elevate Your Transdermal Research with Enokon
Precise simulation is the key to successful drug delivery. As a leading manufacturer and trusted partner in transdermal solutions, Enokon provides the expertise you need to transition from laboratory testing to market-ready products.
We offer a comprehensive range of transdermal drug delivery products, including Lidocaine, Menthol, Capsicum, Herbal, and Far Infrared pain relief patches, as well as specialized solutions like Eye Protection, Detox, and Medical Cooling Gel patches.
Whether you are looking for wholesale transdermal patches or need customized R&D and manufacturing for your unique formulation (excluding microneedles), our team is ready to support your goals.
Contact Enokon Today for Expert Transdermal Solutions
References
- Degong Yang, Liang Fang. The molecular design of drug-ionic liquids for transdermal drug delivery: Mechanistic study of counterions structure on complex formation and skin permeation. DOI: 10.1016/j.ijpharm.2021.120560
This article is also based on technical information from Enokon Knowledge Base .
Related Products
People Also Ask
- How do advanced R&D in transdermal patch manufacturing improve patient tolerance? Enhancing Perioperative Care Solutions
- What functional roles does the backing layer of a transdermal patch perform? More Than Just Support
- What role does the protective backing layer play in transdermal patches? Essential Guide to Drug Stability & Delivery
- What are the advantages and disadvantages of high-permeability silicone membranes in 5-layer transdermal films?
- Why do silicone pressure-sensitive adhesives often demonstrate higher transdermal flux? Boost Drug Delivery Efficiency