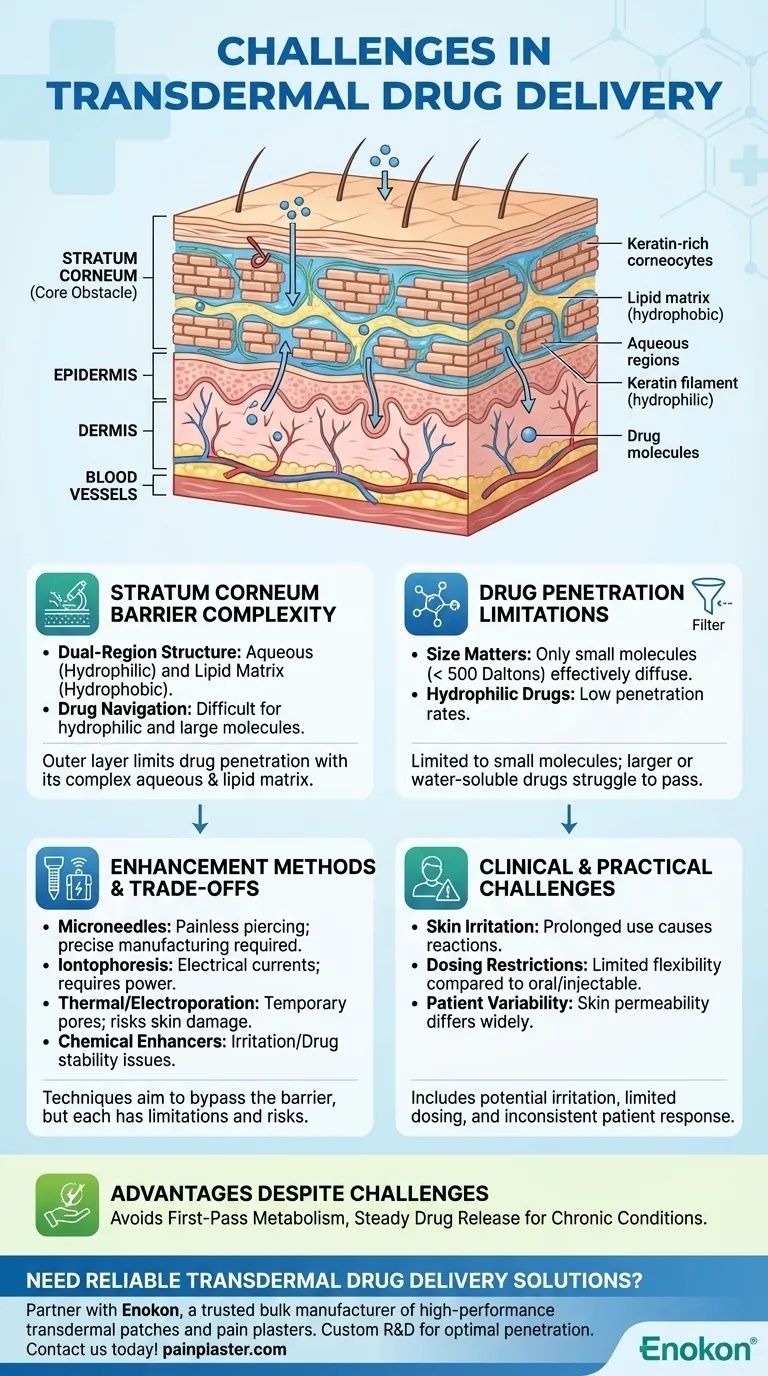
The primary challenge in transdermal drug delivery is overcoming the skin's natural barrier, particularly the stratum corneum, which consists of keratin-rich corneocytes and a dual-region structure (aqueous and lipid matrix) that limits drug penetration. Modern enhancement methods like microneedles, iontophoresis, and thermal poration aim to address this, but limitations persist regarding drug types (small molecules only) and potential skin irritation. Proper application techniques and site rotation can mitigate some issues, but the fundamental barrier remains the core obstacle.

Key Points Explained:
-
Stratum Corneum Barrier Complexity
- The stratum corneum is the outermost skin layer and the main barrier to drug delivery. Its structure includes:
- Keratin-heavy corneocytes that create a dense physical barrier.
- Two chemically distinct regions:
- Aqueous regions at keratin filament surfaces (hydrophilic).
- Lipid matrix between filaments (hydrophobic).
- Drugs must navigate both regions, which is particularly challenging for hydrophilic or large-molecule medications. Transdermal drug patches often struggle with this dual-path requirement.
- The stratum corneum is the outermost skin layer and the main barrier to drug delivery. Its structure includes:
-
Drug Penetration Limitations
- Only small-molecule drugs (typically < 500 Daltons) can effectively diffuse through the skin.
- Hydrophilic drugs face low penetration rates due to the lipid-dominated matrix.
- Variability in skin thickness and composition (e.g., age, ethnicity, hydration) further complicates consistent delivery.
-
Enhancement Methods and Their Trade-offs
Modern techniques aim to bypass or disrupt the stratum corneum:- Microneedles: Painlessly pierce the barrier but require precise manufacturing.
- Iontophoresis: Uses electrical currents to drive charged drugs, yet demands power sources.
- Thermal/Eletroporation: Creates temporary pores but risks localized skin damage.
- Chemical Enhancers: May irritate skin or alter drug stability.
- Ultrasound: Disrupts the barrier non-invasively but lacks precision.
-
Clinical and Practical Challenges
- Skin Irritation: Prolonged patch use can cause mild reactions (redness, itching), though proper rotation and clean application reduce risks.
- Dosing Restrictions: Unlike oral or injectable routes, transdermal delivery offers limited dose flexibility.
- Patient Variability: Skin permeability differs widely, requiring personalized adjustments.
-
Advantages Despite Challenges
- Avoids first-pass liver metabolism, reducing side effects like stomach upset.
- Provides steady drug release, ideal for chronic conditions (e.g., nicotine or hormone patches).
Have you considered how advancements in nanotechnology might further bridge the gap in transdermal delivery? Innovations like nanoemulsions or lipid-based carriers are quietly reshaping this field, offering hope for broader drug compatibility.
Summary Table:
| Key Challenge | Details |
|---|---|
| Stratum Corneum Barrier | Dual-region structure (aqueous/lipid) limits drug penetration. |
| Drug Limitations | Small molecules (<500 Daltons) only; hydrophilic drugs struggle. |
| Enhancement Methods | Microneedles, iontophoresis, thermal poration—each with trade-offs. |
| Clinical Challenges | Skin irritation, dosing restrictions, patient variability. |
| Advantages | Avoids liver metabolism; steady release for chronic conditions. |
Need reliable transdermal drug delivery solutions? Partner with Enokon, a trusted bulk manufacturer of high-performance transdermal patches and pain plasters. Our expertise in custom R&D ensures optimal drug penetration and patient comfort. Contact us today to discuss tailored solutions for your pharmaceutical or healthcare brand!
Visual Guide
Related Products
- Heating Pain Relief Patches for Menstrual Cramps
- Medical Cooling Gel Patches for Fever Cooling Patches
- Far Infrared Deep Heat Relief Patches Medicated Pain Relief Patches
- Capsaicin Chili Medicated Pain Relief Patches
- Far Infrared Heat Pain Relief Patches Transdermal Patches
People Also Ask
- What is clonidine transdermal used for? A Guide to Weekly Blood Pressure Control
- What serious side effects can the selegiline transdermal patch cause? Recognize Life-Threatening Risks
- How does the rotigotine transdermal system work? A Guide to Continuous 24-Hour Delivery
- What role does the two-chamber vertical Franz diffusion cell play? Optimize Transdermal Drug Permeation Accuracy
- How is a TEWL meter used to evaluate transdermal formulations? Assessing Skin Barrier Integrity and Safety
- What medical problems may affect the use of testosterone transdermal patch? Key Risks & Safety Guide
- How should oxybutynin patches be stored and disposed? A Guide to Medication Safety
- What are the technical advantages of using a laboratory coating machine equipped with a Doctor Knife? Master Precision




