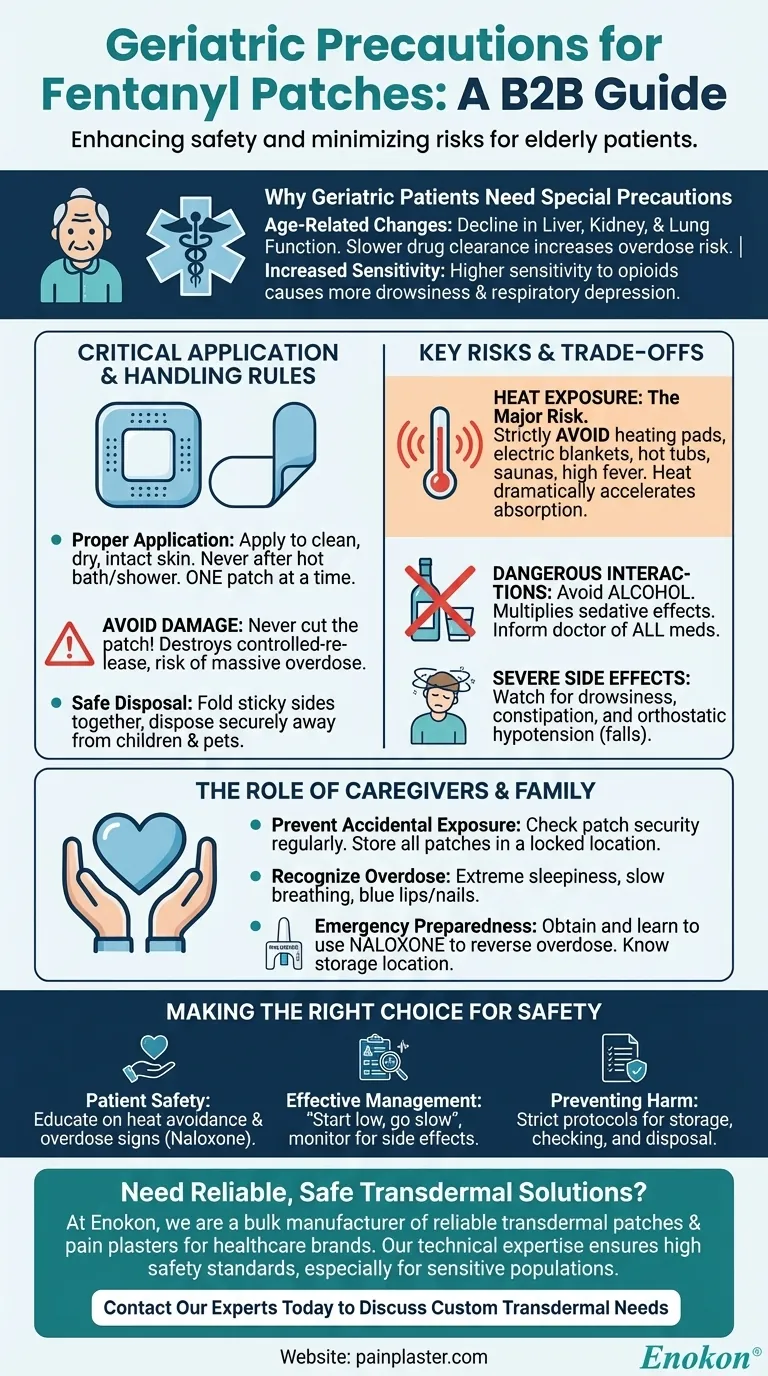
For elderly patients, the primary precautions for fentanyl patches involve starting with a lower dose, strictly avoiding any heat exposure to the patch, and diligently monitoring for increased drowsiness or breathing problems. Age-related changes in organ function mean the body processes the medication more slowly, significantly raising the risk of accidental overdose.
The core issue is that age-related decline in liver, kidney, and lung function makes geriatric patients highly sensitive to fentanyl. This reduced ability to clear the drug means that standard practices, especially heat exposure, can quickly lead to life-threatening respiratory depression.

Why Geriatric Patients Require Special Fentanyl Precautions
Understanding the physiological reasons for these precautions is the first step toward safe use. An elderly body responds to powerful medications like fentanyl very differently than a younger one.
Age-Related Physiological Changes
As people age, the function of their liver and kidneys naturally declines. These organs are critical for processing and clearing medications from the body.
Slower clearance means the drug stays active in their system for longer, which can lead to a dangerous accumulation of fentanyl over time, even with a stable dose.
Increased Sensitivity to Opioids
Geriatric patients are often more sensitive to the central nervous system effects of opioids. This manifests as more pronounced drowsiness, confusion, and dizziness.
Most importantly, this heightened sensitivity creates a greater risk of respiratory depression, a serious side effect where breathing becomes dangerously slow and shallow.
The Necessity of Dose Adjustments
Due to these factors, physicians must almost always adjust the fentanyl dose for an elderly patient. The guiding principle is "start low and go slow."
Initial doses will be conservative, and any increases will be made gradually while closely monitoring the patient's response and any adverse effects.
Critical Application and Handling Rules
Proper handling is not just a suggestion; it is a critical safety measure to prevent overdose for both the patient and those around them.
Proper Patch Application
The patch should only be applied to clean, dry, and intact skin. It should never be applied immediately after a hot bath or shower, as the increased skin temperature will accelerate drug absorption.
Unless specifically instructed by a doctor, never apply more than one patch at a time.
The Danger of Damaging the Patch
A fentanyl patch is designed to release medication slowly over 72 hours. Cutting or damaging the patch destroys this controlled-release system.
This can cause a massive, unregulated dose of fentanyl to be released at once, leading to a rapid and potentially fatal overdose.
Safe Handling and Disposal
Always wash your hands with water immediately after applying a patch. Avoid touching your eyes, nose, or mouth while handling it.
Used patches still contain a significant amount of potent medication. They must be folded with the sticky sides together and disposed of safely, keeping them far out of reach of children and pets.
Understanding the Key Risks and Trade-offs
The benefits of pain relief must be constantly weighed against the significant risks, which are amplified in the elderly population.
The Overdose Risk from Heat Exposure
This is the single most critical environmental precaution. Exposing the patch to any direct heat source—such as a heating pad, electric blanket, hot tub, or sauna—dramatically increases the rate of drug absorption through the skin.
Even a high fever can increase absorption and elevate the risk of an overdose. Any patient with a fever needs to be monitored very closely.
Dangerous Interactions
Alcohol must be strictly avoided, as it multiplies the sedative effects of fentanyl and can lead to severe respiratory depression.
It is essential to inform the prescribing doctor of all other medications, supplements, and over-the-counter drugs being taken to prevent dangerous interactions.
Potential for Severe Side Effects
Beyond drowsiness, be vigilant for side effects like constipation, which can be severe in older adults, and orthostatic hypotension, which is dizziness upon standing that increases the risk of falls.
The Role of Caregivers and Family
Family members and caregivers are the front line of defense in ensuring patient safety. Their vigilance is paramount.
Preventing Accidental Exposure
A patch can partially or fully detach from the patient and adhere to someone else, such as a caregiver or a child sharing a bed. This accidental exposure can be fatal, especially for a child.
Regularly check to ensure the patch is secure and store new and used patches in a locked, secure location.
Recognizing Overdose Symptoms
Everyone in the home should know how to recognize the signs of an opioid overdose. Key symptoms include extreme sleepiness, inability to wake up, very slow or shallow breathing, and blue-tinted lips or fingernails.
Preparing for an Emergency with Naloxone
Caregivers and family should ask the doctor or pharmacist for a prescription for naloxone. This is a life-saving medication that can temporarily reverse the effects of an opioid overdose.
Ensure everyone knows where the naloxone is stored and how to administer it before emergency medical help arrives.
Making the Right Choice for Your Goal
Vigilance and education are the keys to managing pain with fentanyl patches safely in a geriatric patient.
- If your primary focus is patient safety: Prioritize educating the patient and all caregivers on the absolute avoidance of heat, the signs of overdose, and how to use naloxone.
- If your primary focus is effective pain management: Insist on a "start low, go slow" dosing strategy and maintain open communication with the provider about both pain levels and any side effects, especially drowsiness or confusion.
- If your primary focus is preventing harm to others: Implement strict protocols for patch storage, checking for adhesion, and immediate, safe disposal of used patches.
Ultimately, using this powerful medication safely hinges on a clear understanding of the heightened risks and a disciplined commitment to proven safety protocols.
Summary Table:
| Precaution | Key Action | Why It's Critical for Geriatrics |
|---|---|---|
| Dosing | Start low, go slow | Slower drug clearance increases overdose risk |
| Heat Exposure | Strictly avoid heating pads, hot baths | Heat accelerates absorption, causing overdose |
| Monitoring | Watch for drowsiness, breathing issues | Higher sensitivity to respiratory depression |
| Patch Handling | Never cut; secure disposal | Damaged patches release fatal doses |
| Caregiver Role | Learn naloxone use; check adhesion | Prevents accidental exposure and overdose |
Need Reliable, Safe Transdermal Solutions for Your Geriatric Patients?
At Enokon, we are a bulk manufacturer of reliable transdermal patches and pain plasters for healthcare distributors and pharmaceutical brands. Our technical expertise ensures your products are developed with the highest safety standards, especially for sensitive populations like the elderly.
Benefit from our custom R&D to create patches with precise dosing and controlled release, minimizing risks for geriatric users. Let's collaborate to develop safer pain management solutions.
Contact our experts today to discuss your custom transdermal patch needs.
Visual Guide
Related Products
- Icy Hot Menthol Medicine Pain Relief Patch
- Menthol Gel Pain Relief Patch
- Far Infrared Deep Heat Relief Patches Medicated Pain Relief Patches
- Asthma Cough and Pain Relief Patch for Adults and Kids
- Mugwort Wormwood Pain Relief Patch for Neck Pain
People Also Ask
- Can cooling patches be used on newborns? Safe Fever Relief for Infants
- How should a menthol patch be applied? Follow These Steps for Safe & Effective Pain Relief
- How does menthol work in the Reliever Patch? Dual-Action Pain Relief Explained
- What are the important warnings for using menthol topical? Safety Tips for Effective Pain Relief
- Is menthol topical safe during pregnancy and breastfeeding? Key Safety Insights