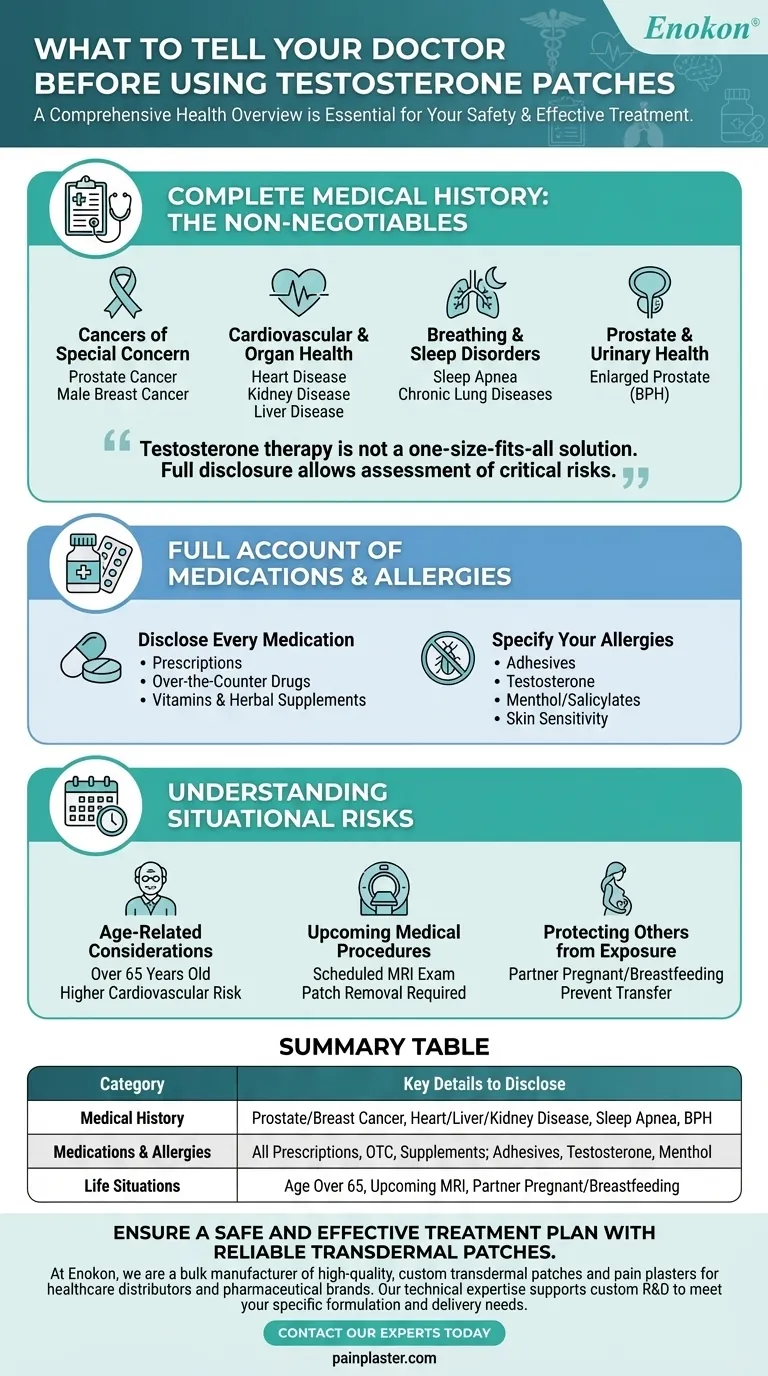
Before starting testosterone patches, a comprehensive health overview is essential for your safety. You must inform your doctor about your complete medical history, paying special attention to any history of prostate or breast cancer, heart, liver, or kidney disease, and sleep apnea. It is also critical to provide a full list of all current medications and disclose any known allergies, especially to adhesives or the medication itself.
Testosterone therapy is not a one-size-fits-all solution. Full disclosure of your health profile allows your doctor to assess critical risks, prevent dangerous interactions, and determine if the potential benefits truly outweigh the known hazards for your specific situation.

Your Complete Medical History: The Non-Negotiables
Providing a thorough medical history is the most important step you can take. Certain conditions can be significantly worsened by testosterone therapy, making it a potentially dangerous choice for some individuals.
Cancers of Special Concern
You must report any personal or family history of prostate cancer or male breast cancer. These conditions are often sensitive to hormones, and testosterone therapy could potentially accelerate their growth.
Cardiovascular and Organ Health
Inform your doctor if you have ever been diagnosed with heart disease, kidney disease, or liver disease. Testosterone can cause the body to retain salt and water, which can increase strain on these vital organs and worsen existing conditions.
Breathing and Sleep Disorders
A history of sleep apnea is a critical piece of information. Testosterone can exacerbate this condition, leading to more frequent or severe interruptions in breathing during sleep. Also mention any other chronic lung diseases, like asthma.
Prostate and Urinary Health
If you have a history of an enlarged prostate, also known as Benign Prostatic Hyperplasia (BPH), you must discuss it. Testosterone can worsen urinary symptoms associated with an enlarged prostate, such as difficulty urinating.
A Full Account of Medications and Allergies
Interactions and allergic reactions are preventable risks, but only with full transparency. Your doctor needs a complete picture to avoid complications.
Disclose Every Medication
Provide a complete list of everything you take. This includes all prescription medications, over-the-counter drugs (like aspirin), vitamins, and herbal supplements.
Specify Your Allergies
Report any and all allergies. This is crucial not only for testosterone itself but also for the adhesives used in the patch. Some patches may contain other ingredients like menthol or salicylates, so report any sensitivity to these as well.
Understanding the Situational Risks
Beyond your baseline health, certain life circumstances and planned events require specific discussion with your doctor to ensure your safety and the safety of others.
Age-Related Considerations
If you are over 65 years old, it is important to have an explicit conversation about the risks versus the benefits. The potential for cardiovascular side effects can be higher in older adults.
Upcoming Medical Procedures
You must inform your medical team if you have a scheduled MRI exam. Some patches contain metal components that can overheat during an MRI and cause serious skin burns. The patch must be removed beforehand. Similarly, inform any surgeon of your patch use before a procedure.
Protecting Others from Exposure
If your partner is pregnant, trying to become pregnant, or breastfeeding, this is a critical detail to share. The testosterone from the patch can be transferred through skin contact and can be harmful to a developing fetus or a baby.
Preparing for Your Doctor's Appointment
To ensure a safe and productive conversation, be prepared to discuss your health honestly and completely.
- If you have a history of prostate or breast cancer: You must inform your doctor immediately, as testosterone therapy is often not recommended.
- If you suffer from sleep apnea, heart, or kidney disease: Be prepared to discuss how testosterone might worsen these conditions and what monitoring will be required.
- If you are taking other medications or have known allergies: Arrive with a complete, written list to prevent dangerous drug interactions or skin reactions.
- If your partner could become pregnant or you have an upcoming MRI: Mention these life factors to establish a plan for preventing transference or injury.
A transparent conversation with your doctor is the first and most critical step toward safe and effective treatment.
Summary Table:
| Information Category | Key Details to Disclose |
|---|---|
| Medical History | Prostate/breast cancer, heart/liver/kidney disease, sleep apnea, enlarged prostate (BPH). |
| Medications & Allergies | All prescriptions, OTC drugs, supplements; allergies to adhesives, testosterone, or menthol. |
| Life Situations | Age over 65, upcoming MRI, partner who is pregnant/breastfeeding. |
Ensure a safe and effective treatment plan with reliable transdermal patches. At Enokon, we are a bulk manufacturer of high-quality, custom transdermal patches and pain plasters for healthcare distributors and pharmaceutical brands. Our technical expertise supports custom R&D to meet your specific formulation and delivery needs. Contact our experts today to discuss how we can partner on your next project. Get in Touch
Visual Guide
Related Products
- Prostate Pain Kidney Health Care Patch for Men
- Capsaicin Chili Medicated Pain Relief Patches
- Far Infrared Deep Heat Relief Patches Medicated Pain Relief Patches
- Heating Pain Relief Patches for Menstrual Cramps
- Herbal Eye Protection Patch Eye Patch
People Also Ask
- How often should testosterone patches be applied? Daily Dosage & Best Practices
- What is the purpose of testosterone patches? A Steady Solution for Low Testosterone
- What lifestyle factors should be considered when choosing between testosterone patches and injections? Find Your Best Fit
- What should be done in case of a testosterone patch overdose? A Step-by-Step Emergency Guide
- What should be done before undergoing an MRI while using testosterone patches? Remove it to prevent serious burns.













