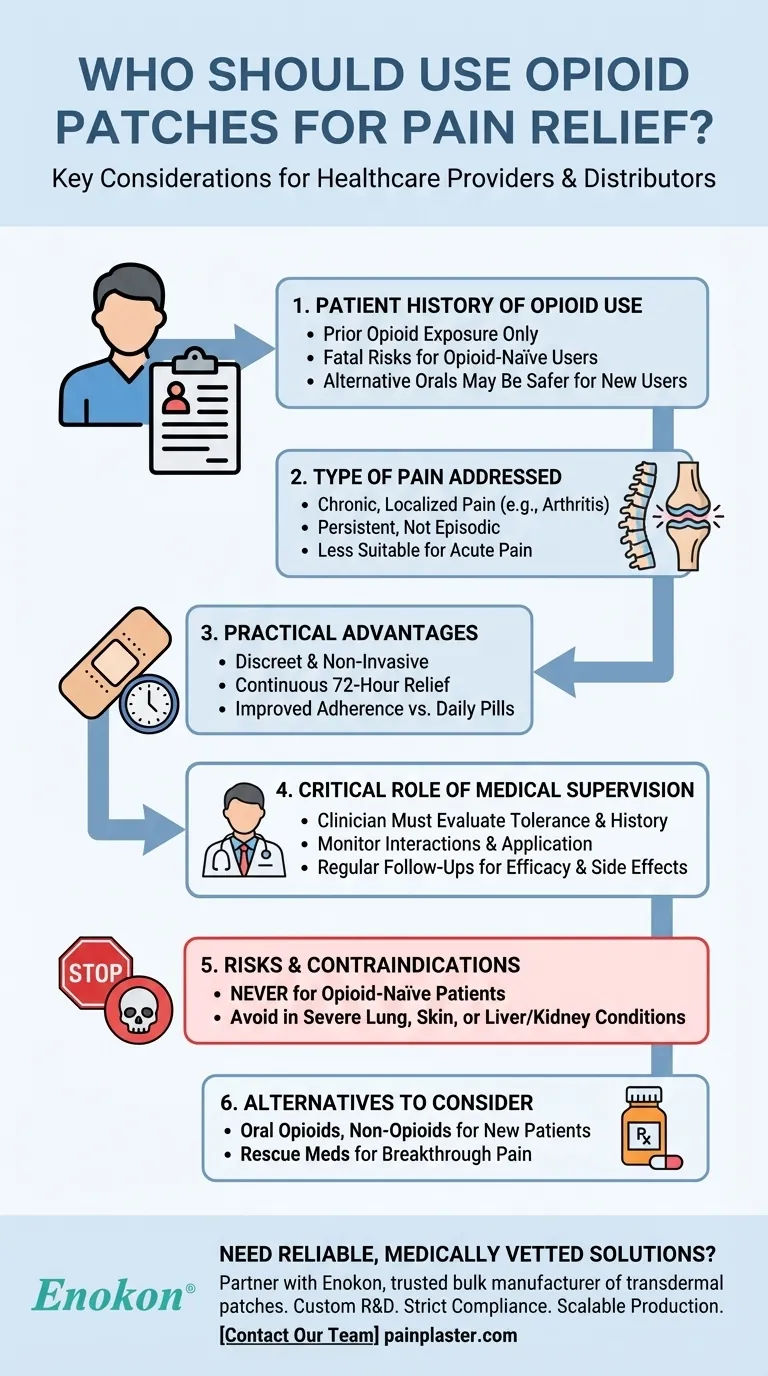
Opioid patches, a type of medicated patches, are designed for specific patient populations under strict medical supervision. They are not suitable for everyone and should only be used by individuals with a documented history of opioid use, as opioid-naïve patients face severe risks, including fatal outcomes. These patches are ideal for managing persistent, localized pain, providing discreet and continuous relief, particularly for those needing mobility or overnight comfort. The decision to use opioid patches must always involve a healthcare professional to assess suitability and safety.

Key Points Explained:
-
Patient History of Opioid Use
- Opioid patches should only be prescribed to patients with prior opioid exposure.
- Opioid-naïve individuals (no prior use) risk life-threatening respiratory depression or overdose due to the patches' sustained drug release.
- Alternative oral opioids (e.g., morphine pills) may be safer for new users, but this requires professional evaluation.
-
Type of Pain Addressed
- Best for chronic, localized pain (e.g., arthritis, neuropathy) that is persistent and not episodic.
- Patches provide steady medication delivery, avoiding peaks and troughs associated with oral doses.
- Less suitable for acute or fluctuating pain, where rapid dose adjustments are needed.
-
Practical Advantages
- Discreet and non-invasive: Ideal for patients who dislike pills or need uninterrupted relief during activities/sleep.
- Reduced dosing frequency: Typically applied every 72 hours, improving adherence compared to multiple daily pills.
-
Critical Role of Medical Supervision
- A clinician must evaluate:
- Patient’s opioid tolerance and medical history.
- Potential drug interactions (e.g., sedatives increasing overdose risk).
- Proper application (e.g., avoiding heat exposure that accelerates drug release).
- Regular follow-ups to monitor efficacy and side effects (e.g., skin irritation, dizziness).
- A clinician must evaluate:
-
Risks and Contraindications
- Never for opioid-naïve patients: Even low-dose patches can cause fatal respiratory depression in this group.
- Avoid in patients with:
- Severe asthma or lung conditions.
- Skin disorders at the application site.
- Liver/kidney impairment affecting drug metabolism.
-
Alternatives to Consider
- For new pain patients: Oral opioids or non-opioid options (e.g., NSAIDs, physical therapy).
- For breakthrough pain: Rescue medications (short-acting opioids) alongside patches, if prescribed.
Opioid patches are a powerful tool for select patients, blending convenience with controlled relief. Yet, their misuse can be deadly—underscoring why professional guidance is non-negotiable. Have you discussed your pain management plan with a provider who understands your full medical history?
Summary Table:
| Key Consideration | Details |
|---|---|
| Patient History | Only for those with prior opioid exposure; fatal risks for opioid-naïve users. |
| Pain Type | Chronic, localized pain (e.g., arthritis); less suitable for acute pain. |
| Advantages | Discreet, continuous relief; reduced dosing frequency (every 72 hours). |
| Medical Supervision | Mandatory clinician evaluation for safety, interactions, and application. |
| Contraindications | Avoid in opioid-naïve patients, severe lung conditions, or skin disorders. |
| Alternatives | Oral opioids or non-opioid therapies for new pain patients. |
Need reliable, medically vetted pain relief solutions? Partner with Enokon, a trusted bulk manufacturer of transdermal opioid patches and pain plasters for healthcare distributors and pharma brands. Our expertise ensures:
- Custom R&D for tailored formulations.
- Strict compliance with safety and efficacy standards.
- Scalable production to meet your supply chain needs.
Contact our team to discuss your requirements or explore collaborative opportunities.
Visual Guide
Related Products
- Far Infrared Deep Heat Relief Patches Medicated Pain Relief Patches
- Capsaicin Chili Medicated Pain Relief Patches
- Far Infrared Heat Pain Relief Patches Transdermal Patches
- Far Infrared Pain Patch Relief Pain Reliever for Back
- Medical Cooling Gel Patches for Fever Cooling Patches
People Also Ask
- How do pain relief patches provide targeted relief? Discover the Science Behind Effective Pain Management
- How often should pain relief patches be used? Get the Right Schedule for Targeted Relief
- How does the Deep Heat Back Patch work? A Drug-Free Solution for Targeted Pain Relief
- How do pain relief patches compare to other pain relief methods? Discover Targeted, Long-Lasting Relief
- What are pain relief patches and how are they used? A Guide to Safe, Targeted Relief













