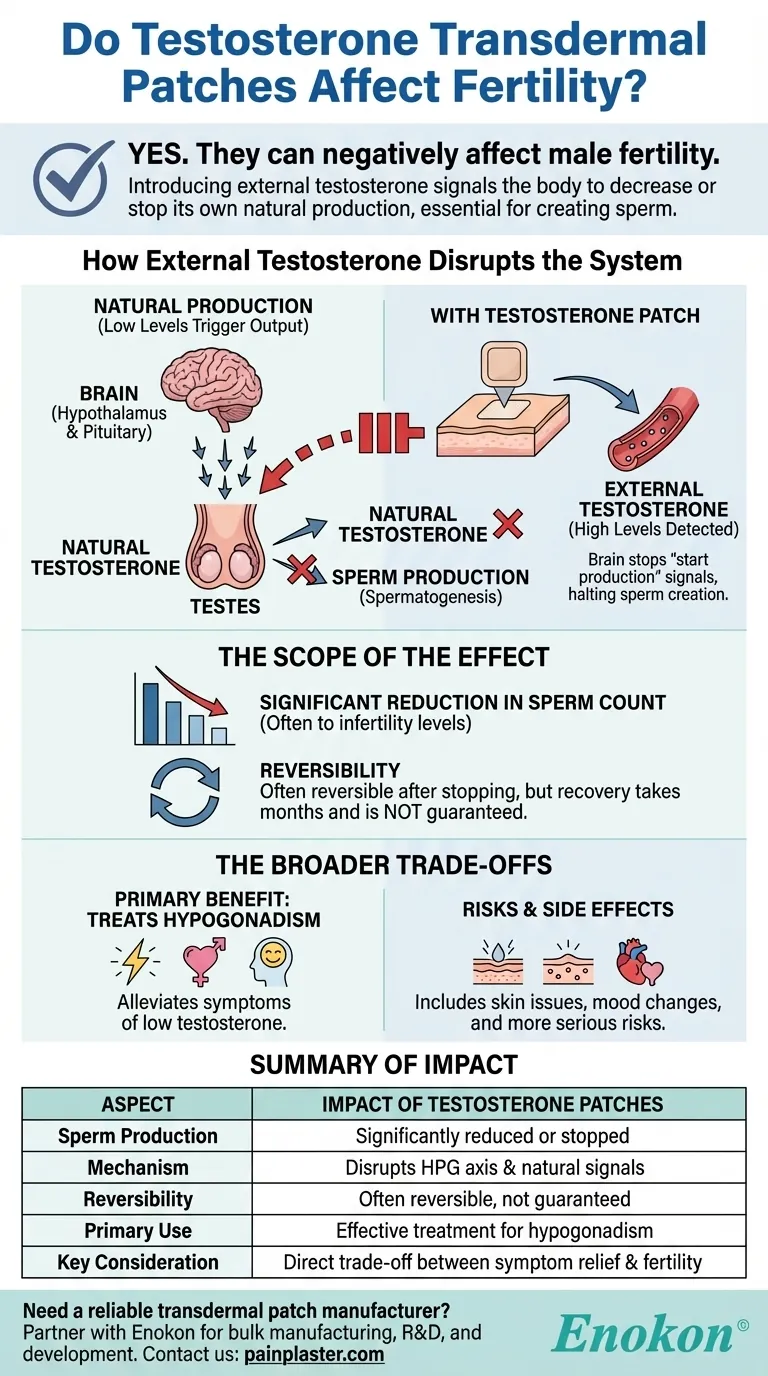
Yes, testosterone transdermal patches can negatively affect male fertility. This occurs because introducing testosterone from an external source, like a patch, signals your body to decrease or completely stop its own natural production, which is essential for creating sperm.
The core issue is a biological feedback loop: providing your body with external testosterone to treat symptoms of hypogonadism simultaneously shuts down the internal machinery required for sperm production. This is a fundamental trade-off that must be discussed with your physician if you are planning to have children.

Why Testosterone Therapy Impacts Sperm Production
The Body's Hormonal Feedback System
Your body's hormone production is managed by a sensitive system called the Hypothalamic-Pituitary-Gonadal (HPG) axis. Think of it as a thermostat for your hormones.
The brain (hypothalamus and pituitary gland) constantly monitors testosterone levels. When levels are low, it sends signals to the testes, telling them to produce more testosterone and to create sperm.
How External Testosterone Disrupts the System
When you apply a testosterone patch, you are introducing the hormone directly into your bloodstream. Your brain detects these higher levels and assumes the testes are overproducing.
In response, it stops sending the "start production" signals. This effectively turns off the testes' dual functions: natural testosterone production and sperm production (a process called spermatogenesis).
The Scope of the Effect on Fertility
A Common and Significant Reduction
The decrease in sperm production is not a rare side effect; it is a predictable physiological response to testosterone replacement therapy (TRT).
For many men on TRT, sperm counts can drop significantly, sometimes to levels that result in infertility.
Is the Effect Permanent?
In most cases, the effect on fertility is reversible. Once testosterone therapy is stopped, the brain typically resumes sending signals to the testes, and sperm production can recover over a period of several months.
However, recovery is not guaranteed for everyone, and the time it takes can vary widely. Pre-existing fertility issues can complicate this recovery process.
Understanding the Broader Trade-offs
The Primary Benefit: Treating Hypogonadism
Testosterone patches are a prescribed medical treatment for men with clinically diagnosed hypogonadism—a condition where the body does not produce enough testosterone on its own.
The goal is to alleviate symptoms like low energy, decreased libido, and mood changes, which can significantly impact quality of life.
The Associated Risks and Side Effects
Beyond fertility, using testosterone patches involves other potential side effects that you must be aware of.
Common issues include skin irritation, blistering, or redness at the application site. Other possible effects are acne, enlarged breasts, and mood changes like depression or irritability.
Serious Health Considerations
More serious, though less common, risks exist. These include an increased risk of blood clots, potential heart problems, and a possible increased risk of prostate issues.
Any symptoms like chest pain, shortness of breath, leg swelling, or difficulty urinating require immediate medical attention.
Making the Right Choice for Your Goal
Before starting or continuing treatment, it is critical to align the therapy with your personal life goals. This requires a frank discussion with your doctor.
- If your primary focus is preserving fertility to have children: Discuss alternatives to testosterone patches with your doctor, as this treatment directly compromises sperm production.
- If your primary focus is treating the symptoms of low testosterone and fertility is not a current concern: Use the patch exactly as prescribed, rotate application sites to minimize skin irritation, and remain vigilant for any potential side effects.
Ultimately, managing low testosterone while considering family planning requires a proactive and informed conversation with your healthcare provider.
Summary Table:
| Aspect | Impact of Testosterone Patches |
|---|---|
| Sperm Production | Significantly reduced or stopped |
| Mechanism | Disrupts the HPG axis, halting natural signals for spermatogenesis |
| Reversibility | Often reversible after stopping treatment, but not guaranteed |
| Primary Use | Effective treatment for symptoms of hypogonadism (low testosterone) |
| Key Consideration | A direct trade-off between symptom relief and fertility |
Need a reliable transdermal patch manufacturer?
If you are a healthcare or pharma distributor or brand developing hormone therapies or other transdermal solutions, partner with Enokon. As a bulk manufacturer of reliable transdermal patches and pain plasters, we offer custom R&D and development expertise to bring your product to market efficiently.
Contact our technical experts today to discuss your project requirements and benefit from our proven manufacturing capabilities.
Visual Guide
Related Products
- Prostate Pain Kidney Health Care Patch for Men
- Far Infrared Heat Pain Relief Patches Transdermal Patches
- Medical Cooling Gel Patches for Fever Cooling Patches
- Hydra Gel Health Care Eye Patch
- Menthol Gel Pain Relief Patch
People Also Ask
- What should someone do if they stop using the patch but do not want to get pregnant? Ensure Uninterrupted Protection
- What is the appropriate patient population for transdermal selegiline? A Guide for Treatment-Resistant Depression
- How does transdermal drug delivery differ from oral administration? Key Benefits & Applications
- How should clonidine patches be stored and disposed of? Essential Safety Guide to Prevent Accidents
- What conditions should be reported before using testosterone patches? Ensure Safe Hormone Therapy
- How should nicotine patches be stored? Ensure Potency and Safety for Effective Quitting
- What are potential side effects of clonidine transdermal? Managing Skin Reactions & Systemic Risks
- What factors contribute to skin irritation from transdermal patches? Uncover the 4 Key Causes















