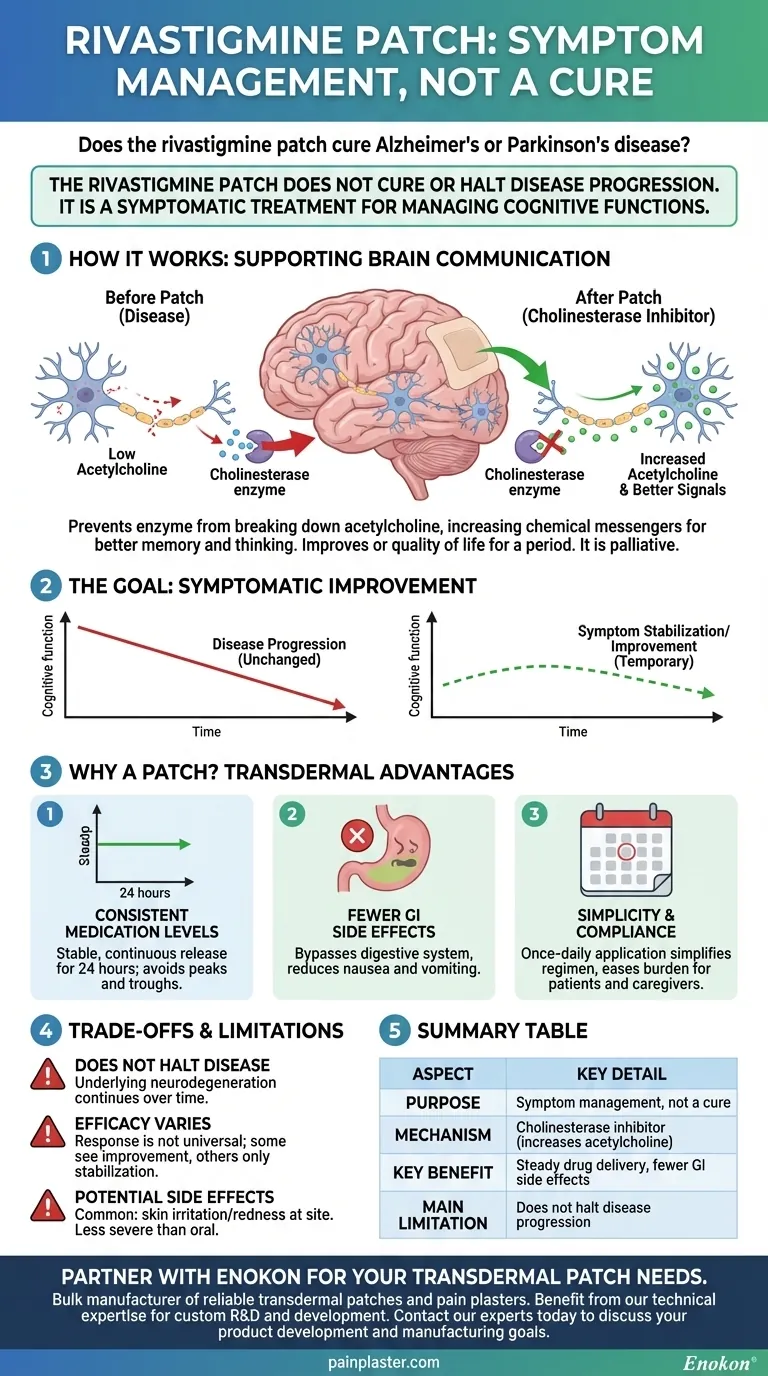
To be clear, the rivastigmine patch does not cure Alzheimer's disease or the dementia associated with Parkinson's disease. Its purpose is not to reverse or halt the underlying disease process. Instead, it is a symptomatic treatment designed to help manage cognitive functions like memory, thinking, and the ability to perform daily activities.
The rivastigmine patch is a tool for managing symptoms, not a cure. Its primary function is to temporarily improve cognitive function and its main advantage over oral forms is a steadier delivery of medication with potentially fewer side effects.

What the Rivastigmine Patch Actually Does
Understanding this medication requires a shift in perspective from "curing" to "managing." It works by addressing the chemical imbalances in the brain caused by the disease, providing temporary support for cognitive processes.
How It Works: Supporting Brain Communication
Rivastigmine is a type of drug known as a cholinesterase inhibitor. In diseases like Alzheimer's, the brain has lower levels of a chemical called acetylcholine, which is crucial for communication between nerve cells.
This drug works by preventing an enzyme from breaking down acetylcholine. By increasing the amount of this chemical messenger, the patch helps improve the transmission of signals between brain cells, which can lead to improvements in memory and thinking.
The Goal: Symptomatic Improvement
The intended outcome of the patch is to improve or slow the decline of symptoms for a period of time. This can translate into a better ability to perform daily tasks and maintain a higher quality of life.
It is important to understand that this effect is palliative; the patch does not alter the progressive course of the disease itself.
Why a Patch? The Advantages of Transdermal Delivery
The user's question specifically mentions the patch, and for good reason. The delivery method is a key feature of this treatment, designed to overcome some of the challenges of oral medication.
Consistent Medication Levels
A patch delivers the drug through the skin directly into the bloodstream over a 24-hour period. This provides a stable and continuous release of medication, avoiding the peaks and troughs associated with taking pills.
Bypassing the Digestive System
By avoiding the digestive system, the patch can significantly reduce gastrointestinal side effects like nausea and vomiting, which are common with oral cholinesterase inhibitors. This improved tolerability is a major reason it is often prescribed.
Simplicity for Patients and Caregivers
For individuals with memory impairment, remembering to take pills multiple times a day can be a significant challenge. A once-daily patch simplifies the medication regimen, which can improve compliance and is often preferred by caregivers.
Understanding the Trade-offs and Limitations
To make an informed decision, you must have a clear-eyed view of what this treatment cannot do and what its potential downsides are.
It Does Not Halt Disease Progression
This is the most critical point to internalize. The rivastigmine patch does not stop the underlying neurodegeneration. Over time, the disease will continue to advance, and the medication's effectiveness may decrease as brain cells are further damaged.
Efficacy Varies by Individual
The response to rivastigmine is not universal. Some patients experience noticeable improvements in cognitive function, while others may only see a stabilization of their symptoms or experience little benefit.
Potential for Side Effects
While the patch improves tolerability, it is not free of side effects. The most common issue is skin irritation or redness at the application site. Other side effects can still occur, though they are often less severe than with the oral form.
Making the Right Choice for Your Goal
Discussing this treatment with a doctor is essential. The right choice depends entirely on a realistic understanding of your goals.
- If your primary focus is to find a cure: The rivastigmine patch is not the correct tool, as no cure for Alzheimer's or Parkinson's dementia currently exists.
- If your primary focus is to manage cognitive symptoms: The patch is considered an effective first-line therapy for improving memory and daily function in mild to moderate stages of the disease.
- If your primary focus is minimizing medication side effects: The patch's transdermal delivery system is specifically designed to improve tolerability compared to oral forms, making it a valuable option.
Ultimately, the rivastigmine patch is a strategic tool designed to improve quality of life while living with a progressive disease.
Summary Table:
| Aspect | Key Detail |
|---|---|
| Purpose | Symptom management, not a cure |
| Mechanism | Cholinesterase inhibitor (increases acetylcholine) |
| Key Benefit | Steady drug delivery, fewer GI side effects |
| Main Limitation | Does not halt disease progression |
Partner with Enokon for Your Transdermal Patch Needs
As a bulk manufacturer of reliable transdermal patches and pain plasters, Enokon provides healthcare and pharmaceutical distributors and brands with high-quality, consistent drug delivery solutions. Benefit from our technical expertise for custom R&D and development to create effective symptomatic treatments like rivastigmine patches.
Contact our experts today to discuss how we can support your product development and manufacturing goals.
Visual Guide
Related Products
- Herbal Eye Protection Patch Eye Patch
- Far Infrared Deep Heat Relief Patches Medicated Pain Relief Patches
- Asthma Cough and Pain Relief Patch for Adults and Kids
- Menthol Gel Pain Relief Patch
- Icy Hot Menthol Medicine Pain Relief Patch
People Also Ask
- Can under eye patches smooth fine lines and wrinkles? Hydrate & Plump for Youthful Skin
- Should under eye patches be applied before or after moisturizer? Optimize Your Skincare Routine
- How do eye patches enhance the effectiveness of eye creams? Boost Your Eye Care Routine
- What are the main benefits of using eye patches in a skincare routine? Revitalize Your Under-Eye Area
- What are the steps for properly using eye patches? Maximize Benefits for Your Delicate Eye Area
















