For localized pain, transdermal patches work by delivering a high concentration of medication directly through the skin to the nerves in a specific, painful area. This method provides targeted treatment with very little of the drug entering the bloodstream. The most common examples, lidocaine and capsaicin patches, are designed to numb or desensitize nerve endings right at the source of pain, such as with postherpetic neuralgia (pain after a shingles outbreak).
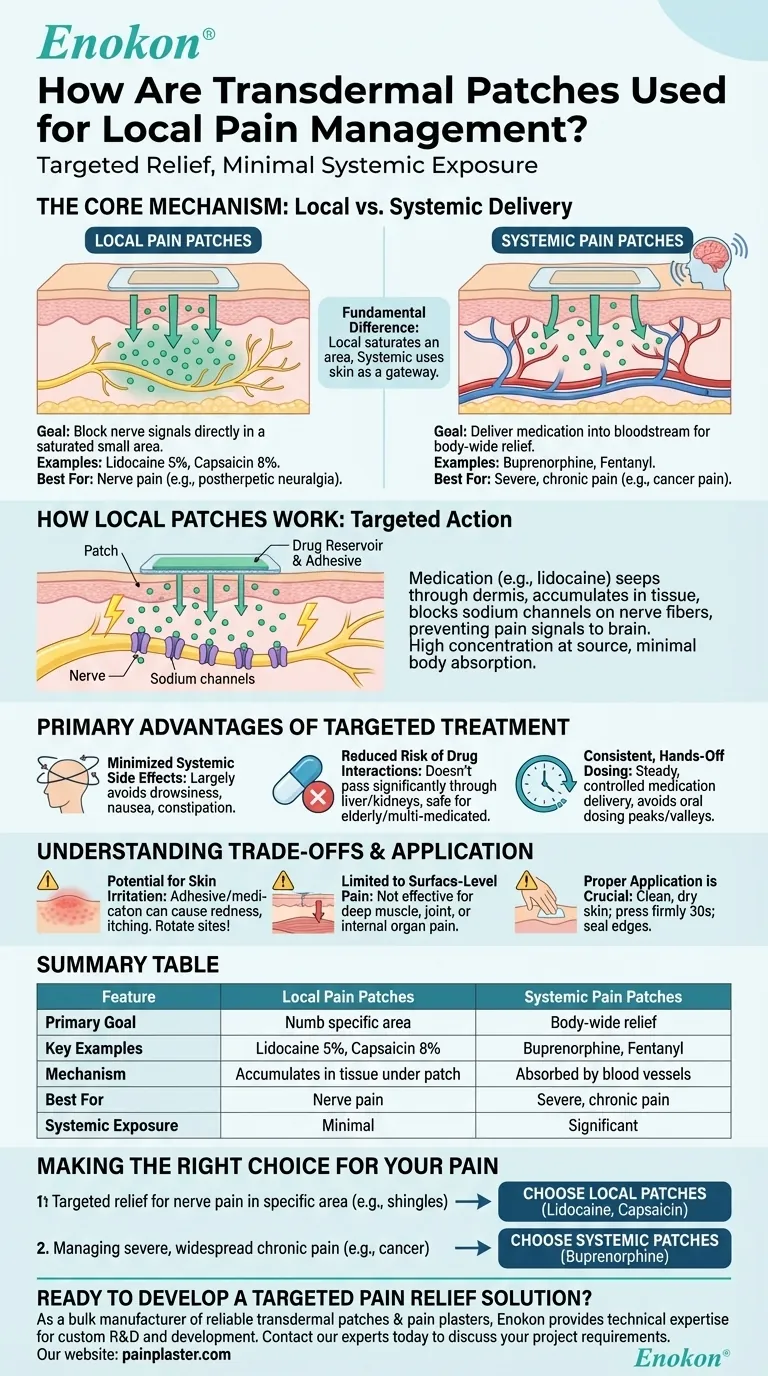
The fundamental difference in transdermal pain patches lies in their goal: patches for local pain saturate a small area to block nerve signals directly, while patches for systemic pain use the skin as a gateway to deliver medication into the bloodstream for body-wide relief.

The Core Mechanism: Local vs. Systemic Delivery
To understand how patches manage local pain, it's crucial to distinguish their function from patches designed for widespread, chronic pain.
How Local Patches Work
A patch for local pain acts as a drug reservoir held against the skin by an adhesive layer.
The medication, such as lidocaine, slowly seeps through the outer layer of skin (the dermis) and accumulates in the tissue directly beneath the patch. It works by blocking the sodium channels in local nerve fibers, preventing them from sending pain signals to the brain.
This creates a high concentration of the analgesic right where it's needed, with minimal absorption into the rest of the body.
How Systemic Patches Differ
In contrast, systemic patches (e.g., buprenorphine or fentanyl) are engineered for the medication to pass through the skin and be absorbed by blood vessels.
The goal here is to achieve a steady, continuous level of the drug in the bloodstream to manage severe, widespread pain, such as that from cancer. They treat the entire body, not just one specific spot.
Key Examples of Local Pain Patches
Two primary medications are used in patches for targeted, local pain relief:
- Lidocaine 5% Patch: This patch delivers a local anesthetic that numbs the area it covers, providing relief from nerve pain conditions.
- Capsaicin 8% Patch: Derived from chili peppers, capsaicin works by desensitizing and overwhelming pain-transmitting nerve fibers in a specific area.
The Primary Advantages of Targeted Treatment
Using a patch for local pain offers distinct benefits, especially when compared to oral medications.
Minimized Systemic Side Effects
Because so little of the drug enters the bloodstream, the side effects commonly associated with oral painkillers—such as drowsiness, nausea, and constipation—are largely avoided.
Reduced Risk of Drug Interactions
This approach is particularly valuable for elderly patients or individuals taking multiple medications. Since the drug acts locally, it doesn't pass through the liver or kidneys in significant amounts, reducing the potential for harmful interactions with other drugs.
Consistent, Hands-Off Dosing
A patch delivers a steady, controlled amount of medication over a set period. This avoids the peaks and valleys of oral dosing and eliminates the need to take pills multiple times a day.
Understanding the Trade-offs and Application
While effective, local patches have specific limitations and require proper handling to be safe and effective.
Potential for Skin Irritation
The adhesive or the medication itself can cause redness, itching, or irritation at the application site. This is the most common side effect of any transdermal patch.
Limited to Surface-Level Pain
Local patches are designed for neuropathic (nerve) pain or pain that originates near the surface of the skin. They are not effective for deep muscle pain, joint pain, or pain originating from internal organs.
Proper Application is Crucial
For any patch to work correctly, it must be applied properly. The area should be clean, dry, and free of oils, lotions, or irritation.
Press the patch firmly onto the skin for about 30 seconds, ensuring the edges are sealed. It's critical to rotate the application site with each new patch to prevent significant skin irritation.
Making the Right Choice for Your Pain
The effectiveness of a transdermal patch depends entirely on matching the type of patch to the type of pain.
- If your primary focus is targeted relief for nerve pain in a specific area (like shingles pain): Localized patches like lidocaine or capsaicin are designed for this purpose, offering relief with minimal body-wide side effects.
- If your primary focus is managing severe, widespread chronic pain (like from cancer): Systemic patches that deliver medication like buprenorphine into the bloodstream are the appropriate choice for continuous, body-wide pain management.
Understanding the distinction between local and systemic action is the key to using transdermal patches safely and effectively for pain relief.
Summary Table:
| Feature | Local Pain Patches | Systemic Pain Patches |
|---|---|---|
| Primary Goal | Numb/desensitize nerves in a specific area | Deliver medication into bloodstream for body-wide relief |
| Key Examples | Lidocaine 5%, Capsaicin 8% | Buprenorphine, Fentanyl |
| Mechanism | Drug accumulates in tissue under the patch | Drug absorbed by blood vessels beneath the skin |
| Best For | Nerve pain (e.g., postherpetic neuralgia) | Severe, chronic pain (e.g., cancer pain) |
| Systemic Exposure | Minimal | Significant |
Ready to develop a targeted pain relief solution?
As a bulk manufacturer of reliable transdermal patches and pain plasters, Enokon provides healthcare and pharma distributors and brands with the technical expertise for custom R&D and development. Benefit from our experience to create effective local pain management products for your customers.
Contact our experts today to discuss your project requirements.
Visual Guide
Related Products
- Far Infrared Heat Pain Relief Patches Transdermal Patches
- Lidocaine Hydrogel Pain Relief Patch for Pain Relief
- Heating Pain Relief Patches for Menstrual Cramps
- Herbal Eye Protection Patch Eye Patch
- Icy Hot Menthol Medicine Pain Relief Patch
People Also Ask
- Why is a transdermal patch formulation designed to contain a concentration of API higher than the therapeutic dose?
- Why do spent transdermal patches still pose potential safety risks? Master Safe Disposal for Residual Drugs
- What are the usage instructions for common pain patch types? A Guide to Safe and Effective Pain Relief
- What special considerations apply to transdermal patches? Ensuring Safe and Effective Use
- What are the key functions of the polyester backing film used in transdermal patches? 4 Essential Benefits for Product Performance
- What serious side effects should prompt immediate removal of the granisetron transdermal patch? Know the Red Flags
- What function does vacuum silicone grease serve during the assembly of a Franz diffusion unit? Ensure Data Accuracy
- What role does polarized light microscopy play in evaluating five-layer stacked film experiments for drug solubility?
















