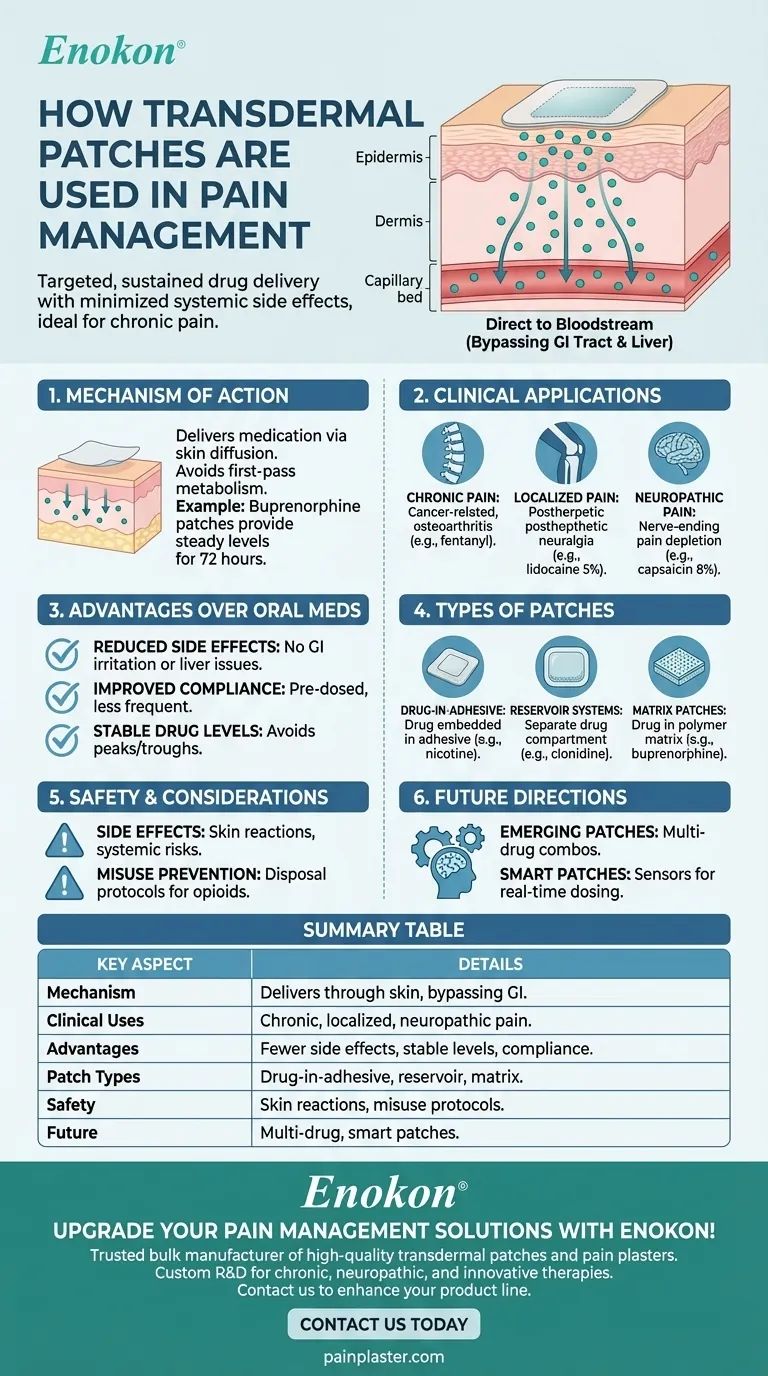
Transdermal patches are a cornerstone in pain management, offering targeted, sustained drug delivery with minimized systemic side effects. They work by releasing analgesics through the skin into the bloodstream, ideal for chronic pain conditions like cancer or neuropathy. Key advantages include bypassing gastrointestinal issues, reducing dosing frequency, and improving patient compliance. Specific formulations like buprenorphine or lidocaine patches address different pain types while maintaining stable drug levels. Their design—ranging from single-layer adhesive to matrix systems—ensures controlled release tailored to clinical needs.

Key Points Explained:
1. Mechanism of Action
- (Transdermal patches)[/topic/transdermal-patch] deliver medication through the skin via diffusion, avoiding first-pass metabolism and gastrointestinal degradation.
- Example: Buprenorphine patches provide steady opioid levels for 72 hours, reducing fluctuations that cause side effects.
2. Clinical Applications in Pain Management
- Chronic Pain: Used for cancer-related pain (e.g., fentanyl patches) and non-malignant conditions (e.g., osteoarthritis).
- Localized Pain: Lidocaine 5% patches target postherpetic neuralgia with minimal systemic absorption.
- Neuropathic Pain: Capsaicin 8% patches deplete nerve-ending pain mediators for sustained relief.
3. Advantages Over Oral Medications
- Reduced Side Effects: No GI irritation (common with NSAIDs) or liver metabolism issues.
- Improved Compliance: Pre-dosed patches eliminate frequent dosing; ideal for elderly or forgetful patients.
- Stable Drug Levels: Avoids peaks/troughs linked to oral dosing, enhancing therapeutic consistency.
4. Types of Transdermal Patches
- Drug-in-Adhesive: Simple design with medication embedded in adhesive (e.g., nicotine patches).
- Reservoir Systems: Separate drug compartment for controlled release (e.g., clonidine for hypertension).
- Matrix Patches: Drug suspended in polymer matrix (e.g., buprenorphine for chronic pain).
5. Safety and Considerations
- Side Effects: Local skin reactions (redness) or systemic risks (e.g., respiratory depression with opioid patches).
- Misuse Prevention: Some patches (like fentanyl) require disposal protocols to prevent accidental exposure.
6. Future Directions
- Emerging patches combine multiple drugs (e.g., opioids + anti-inflammatories) for synergistic effects.
- Smart patches with sensors to adjust dosing based on real-time pain biomarkers are in development.
By integrating these features, transdermal patches exemplify how targeted drug delivery can transform pain management—offering relief that’s as consistent as it is unobtrusive.
Summary Table:
| Key Aspect | Details |
|---|---|
| Mechanism | Delivers medication through skin, bypassing GI tract and liver metabolism. |
| Clinical Uses | Chronic pain (cancer, osteoarthritis), localized pain (lidocaine patches). |
| Advantages | Fewer side effects, stable drug levels, improved patient compliance. |
| Patch Types | Drug-in-adhesive, reservoir systems, matrix patches. |
| Safety | Potential skin reactions; misuse prevention protocols for opioids. |
| Future Innovations | Multi-drug patches, smart patches with sensor-based dosing. |
Upgrade your pain management solutions with Enokon’s transdermal patches!
As a trusted bulk manufacturer, we specialize in high-quality transdermal patches and pain plasters tailored for healthcare distributors and brands. Our expertise in custom R&D ensures formulations that meet your clinical and commercial needs—whether for chronic pain, neuropathic conditions, or innovative combination therapies.
Contact us today to discuss how we can enhance your product line with reliable, patient-friendly transdermal solutions.
Visual Guide
Related Products
- Far Infrared Heat Pain Relief Patches Transdermal Patches
- Heating Pain Relief Patches for Menstrual Cramps
- Capsaicin Chili Medicated Pain Relief Patches
- Medical Cooling Gel Patches for Fever Cooling Patches
- Far Infrared Deep Heat Relief Patches Medicated Pain Relief Patches
People Also Ask
- Are heat patches safe for all body parts? Key Safety Zones and No-Go Areas Explained
- What types of pain can the Deep Heat Pain Relief Back Patch be used for? Targeted Relief for Muscles & Joints
- Can heat patches be used for fresh injuries? Avoid This Common Mistake for Faster Recovery
- How does capsaicin work in the medicated heat patch? The Science Behind Pain Relief
- What are the common side effects of using the medicated heat patch? Understanding Risks & Safe Use
















