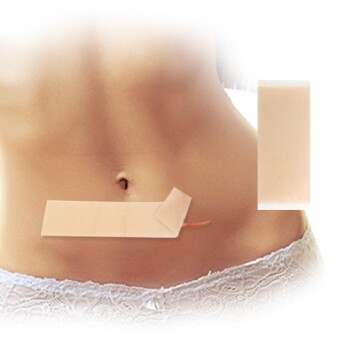
Chemical penetration enhancers (CPEs) act as molecular keys that unlock the skin’s natural defensive barrier, specifically the stratum corneum.
These agents function primarily by temporarily disrupting the highly organized lipid structure of the skin or by altering the solubility of the drug within the skin tissue. By reducing the skin's resistance, enhancers like DMSO, urea, and fatty acids allow larger or highly hydrophobic molecules—which would normally be blocked—to permeate the dermis and reach systemic circulation.
The Core Mechanism The human skin is designed to keep substances out. Chemical enhancers solve this engineering challenge by temporarily compromising the structural integrity of the stratum corneum, creating a window of opportunity for therapeutic agents to pass through the lipid barrier and reach the bloodstream.
Overcoming the Stratum Corneum Barrier
To understand how enhancers work, one must first respect the barrier they are defeating. The stratum corneum acts as the primary rate-limiting step in transdermal drug delivery.
The "Brick and Mortar" Structure
The stratum corneum is often described as a brick-and-mortar structure. The "bricks" are dead skin cells (corneocytes), and the "mortar" consists of highly organized, tightly packed lipid bilayers.
The Challenge of Permeation
Under normal conditions, this lipid mortar is too dense for many drugs to traverse. Large molecules and certain hydrophilic (water-loving) compounds simply bounce off the surface.
The Role of Enhancers
CPEs modify this environment. They do not merely carry the drug; they physically or chemically change the landscape of the skin layers to make them more permeable.
Mechanisms of Action
Chemical enhancers typically utilize three specific methods to increase drug flux (the rate of permeation).
1. Disruption of Lipid Organization
This is the most common mechanism for agents like fatty acids (e.g., oleic or linoleic acid).
These molecules insert themselves into the skin's lipid bilayers. Because they are amphiphilic (containing both oil-loving and water-loving parts), they disrupt the "tight packing" of the natural lipids.
This insertion increases fluidity and disorder within the structure. Imagine loosening the mortar between bricks; the wall remains standing, but gaps appear that allow substances to pass through.
2. Altering Drug Solubility
Agents like DMSO and various organic solvents function by modifying solubility profiles.
For a drug to move from a patch into the skin, it must be soluble within the skin tissue. Enhancers can increase the solubility of the drug specifically within the stratum corneum.
This creates a concentration gradient that drives the drug out of the formulation and into the skin layers, significantly improving permeation efficiency.
3. Extraction and Modification
Some powerful enhancers work by effectively extracting lipids from the stratum corneum or altering protein structures.
By removing or rearranging these barrier components, the resistance of the skin drops significantly. This allows drugs to penetrate both lipophilic and hydrophilic regions of the skin to reach the microvascular network in the dermis.
Specific Agents and Their Functions
While the general goal is the same, different chemicals achieve permeation through slightly different nuances.
Fatty Acids (Oleic and Linoleic Acid)
These primarily work by fluidizing the lipid bilayer. They reduce diffusion resistance, making them particularly effective for lipophilic (fat-loving) drugs that need help navigating the dense lipid environment.
Dimethyl Sulfoxide (DMSO)
DMSO is a potent solvent that alters the barrier properties of the skin. It facilitates the penetration of both lipophilic and hydrophilic drugs by modifying the keratin structure and disrupting lipid organization.
Urea
Urea contributes to hydration and structural disruption. By altering the solubility environment and disrupting lipid arrangements, it assists in opening pathways for drug molecules.
Understanding the Trade-offs
As a technical advisor, it is critical to note that efficacy often comes at a cost.
The Balance of Irritation
The skin barrier exists to protect the body. Any agent that successfully disrupts this barrier to let drugs in may also allow water to get out or irritants to enter.
Reversibility is Critical
The action of a CPE must be temporary. The goal is to reduce barrier resistance only long enough for the drug to be delivered, after which the skin should naturally recover its protective structure.
Formulation Complexity
Adding enhancers changes the chemistry of the patch or gel. Formulators must ensure the enhancer does not degrade the drug or cause the adhesive to fail.
Making the Right Choice for Your Goal
Selecting the right penetration enhancer depends heavily on the physicochemical properties of the drug you are trying to deliver.
- If your primary focus is Lipophilic Drugs: Look for fatty acids (like oleic acid) that insert into bilayers to increase fluidity, reducing the resistance specifically for fat-soluble molecules.
- If your primary focus is Hydrophilic or Large Molecules: Consider solvents like DMSO or alcohols that can significantly alter the solubility profile and open polar pathways through the skin.
- If your primary focus is Safety and Tolerance: Prioritize enhancers with a proven track record of reversible disruption to minimize long-term skin irritation.
The most effective transdermal product is not just the one that delivers the drug, but the one that intelligently navigates the skin's defenses without permanently destroying them.
Summary Table:
| Enhancer Type | Primary Mechanism | Best Suited For |
|---|---|---|
| Fatty Acids (e.g. Oleic Acid) | Disrupts/fluidizes lipid bilayers | Lipophilic (fat-loving) drugs |
| DMSO | Alters solubility and disrupts keratin | Both lipophilic and hydrophilic molecules |
| Urea | Hydrates skin and disrupts lipid structure | Improving polar pathway permeability |
| Solvents | Increases drug concentration gradient | Enhancing flux and drug solubility |
Partner with Enokon for High-Performance Transdermal Solutions
Are you looking to enhance the delivery profile of your next product? Enokon is a trusted brand and manufacturer specializing in wholesale transdermal patches and expert custom R&D solutions. We help you navigate complex formulation challenges to ensure maximum efficacy and skin compatibility.
Our manufacturing capabilities cover a wide range of transdermal products (excluding microneedle technology), including:
- Pain Relief: Lidocaine, Menthol, Capsicum, Herbal, and Far Infrared patches.
- Health & Wellness: Eye Protection, Detox, and Medical Cooling Gel patches.
Take advantage of our technical expertise and scalable production. Contact us today to discuss your custom R&D requirements or wholesale needs!
References
- А.С. Арефьев, И.В. Жукова. ТРАНСДЕРМАЛЬНЫЕ ТЕРАПЕВТИЧЕСКИЕ СИСТЕМЫ, ИХ ТИПЫ И ПРЕИМУЩЕСТВА. DOI: 10.5281/zenodo.6368638
This article is also based on technical information from Enokon Knowledge Base .
Related Products
- Menthol Gel Pain Relief Patch
- Far Infrared Heat Pain Relief Patches Transdermal Patches
- Asthma Cough and Pain Relief Patch for Adults and Kids
- Lidocaine Hydrogel Pain Relief Patch for Pain Relief
- Far Infrared Deep Heat Relief Patches Medicated Pain Relief Patches
People Also Ask
- What precautions should be taken before using a menthol patch? Essential Safety Tips for Effective Relief
- How does menthol work in the Reliever Patch? Dual-Action Pain Relief Explained
- What is the primary use of a menthol patch? Targeted Relief for Muscle & Joint Pain
- What should be done if a dose of menthol patch is missed? Key Steps for Safe Use
- What important precautions should be taken with menthol topical? Safety Guide for Effective Use