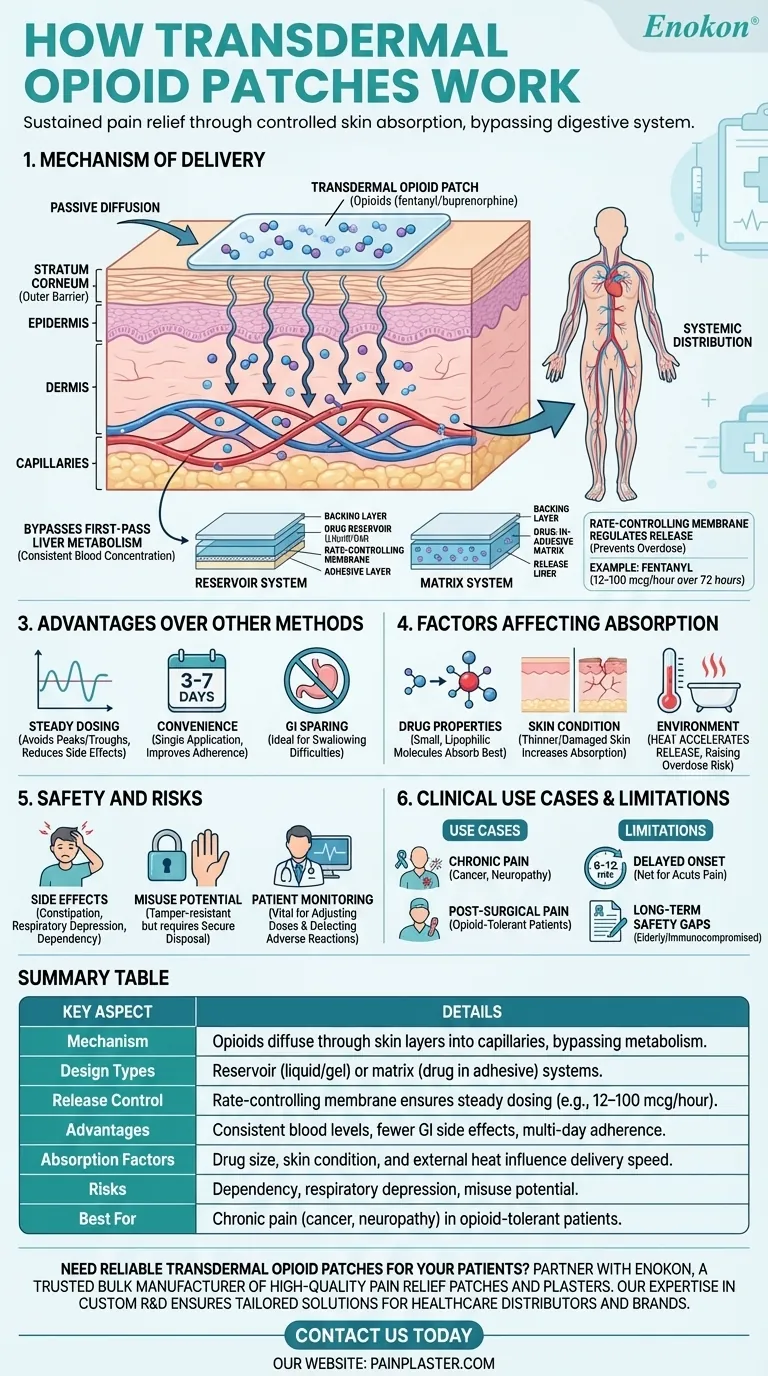
Transdermal opioid patches deliver pain medication through the skin into the bloodstream, offering sustained relief over extended periods. These patches contain opioids like fentanyl or buprenorphine, which are released at controlled rates, bypassing the digestive system and liver metabolism. The drug molecules pass through the skin's layers—stratum corneum, epidermis, and dermis—before entering capillaries for systemic distribution. This method ensures consistent dosing, reduces gastrointestinal side effects, and improves patient compliance. However, factors like molecular size, skin condition, and environmental humidity influence absorption rates. While effective for chronic pain, these patches carry risks similar to other opioids, including dependency and side effects like drowsiness or nausea.

Key Points Explained:
-
Mechanism of Delivery
- The (transdermal patch)[/topic/transdermal-patch] adheres to the skin, releasing opioids through passive diffusion.
- Drug molecules traverse the stratum corneum (outer skin barrier), then the epidermis and dermis, before entering capillaries.
- This bypasses first-pass liver metabolism, ensuring more consistent blood concentration compared to oral opioids.
-
Design and Composition
- Patches use a reservoir (liquid/gel drug storage) or matrix (drug embedded in adhesive) system.
- A rate-controlling membrane or adhesive layer regulates release, preventing overdose.
- Example: Fentanyl patches may deliver 12–100 mcg/hour over 72 hours, tailored to pain severity.
-
Advantages Over Other Methods
- Steady dosing: Avoids peaks/troughs of oral or injectable opioids, reducing side effects like nausea.
- Convenience: Single application lasts days (e.g., 3–7 days per patch), improving adherence.
- GI sparing: Ideal for patients with vomiting or swallowing difficulties.
-
Factors Affecting Absorption
- Drug properties: Small, lipophilic molecules (e.g., fentanyl) absorb best.
- Skin condition: Thinner or damaged skin may increase absorption unpredictably.
- Environment: Heat (e.g., fever, hot baths) can accelerate release, raising overdose risk.
-
Safety and Risks
- Same side effects as other opioids: constipation, respiratory depression, dependency.
- Misuse potential: Patches are tamper-resistant but still require secure disposal.
- Patient monitoring: Vital for adjusting doses and detecting adverse reactions.
-
Clinical Use Cases
- Chronic pain (e.g., cancer, neuropathy) where oral opioids are impractical.
- Post-surgical pain in opioid-tolerant patients (limited to specific formulations).
-
Limitations and Research Gaps
- Not suitable for acute pain due to delayed onset (6–12 hours for full effect).
- More studies needed on long-term safety, especially in elderly or immunocompromised patients.
Have you considered how patch placement (e.g., upper arm vs. torso) might influence absorption rates? These technologies exemplify how subtle engineering—like membrane design—can transform potent drugs into tools that improve quality of life for chronic pain sufferers.
Summary Table:
| Key Aspect | Details |
|---|---|
| Mechanism | Opioids diffuse through skin layers into capillaries, bypassing metabolism. |
| Design Types | Reservoir (liquid/gel) or matrix (drug in adhesive) systems. |
| Release Control | Rate-controlling membrane ensures steady dosing (e.g., 12–100 mcg/hour). |
| Advantages | Consistent blood levels, fewer GI side effects, multi-day adherence. |
| Absorption Factors | Drug size, skin condition, and external heat influence delivery speed. |
| Risks | Dependency, respiratory depression, misuse potential. |
| Best For | Chronic pain (cancer, neuropathy) in opioid-tolerant patients. |
Need reliable transdermal opioid patches for your patients? Partner with Enokon, a trusted bulk manufacturer of high-quality pain relief patches and plasters. Our expertise in custom R&D ensures tailored solutions for healthcare distributors and brands. Contact us today to discuss your requirements and benefit from our technical support!
Visual Guide
Related Products
- Far Infrared Deep Heat Relief Patches Medicated Pain Relief Patches
- Far Infrared Heat Pain Relief Patches Transdermal Patches
- Heating Pain Relief Patches for Menstrual Cramps
- Far Infrared Pain Patch Relief Pain Reliever for Back
- Far Infrared Knee Pain Patch Heat Patches for Pain Relief
People Also Ask
- How do pain relief patches work? A Guide to Targeted, Long-Lasting Pain Relief
- How does the Deep Heat Back Patch work? A Drug-Free Solution for Targeted Pain Relief
- How do pain relief patches compare to other pain relief methods? Discover Targeted, Long-Lasting Relief
- How quickly does the Deep Heat Pain Relief Back Patch activate and how long does it provide warmth? Get 16-Hour Relief
- What are pain relief patches and how are they used? A Guide to Safe, Targeted Relief












