To be direct, testosterone transdermal patches can alter the levels of cholesterol and other fats in your blood. This is a recognized potential side effect that your doctor will monitor as part of your overall treatment plan.
While testosterone therapy can impact your lipid profile, the central issue is not just the change in cholesterol itself, but how this fits into the broader picture of your cardiovascular health and the importance of consistent medical supervision.

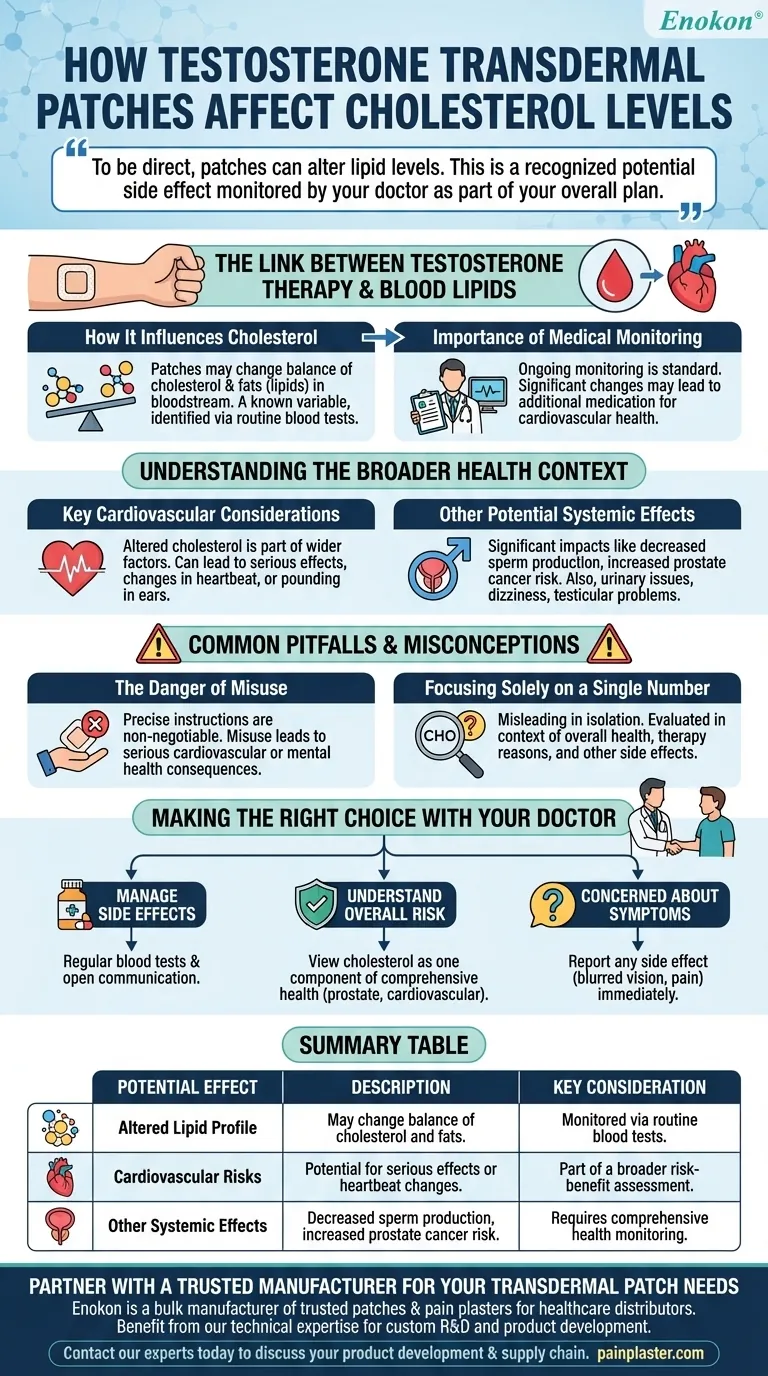
The Link Between Testosterone Therapy and Blood Lipids
When you begin testosterone replacement therapy, it can influence several of your body's systems, including how it processes fats. This requires careful attention from both you and your healthcare provider.
How Testosterone Influences Cholesterol
Testosterone patches may change the balance of different types of cholesterol and other fats, known as lipids, circulating in your bloodstream.
This is a known variable in treatment. If these changes occur, they are typically identified through routine blood tests ordered by your physician.
The Importance of Medical Monitoring
Because of the potential for altered lipid levels, ongoing monitoring is a standard part of testosterone therapy.
If your doctor observes a significant change, they may prescribe additional medication specifically to manage your cholesterol and ensure your cardiovascular health remains protected.
Understanding the Broader Health Context
Focusing only on cholesterol misses the larger picture. Testosterone therapy involves a comprehensive assessment of benefits versus a range of potential risks that extend beyond blood lipids.
Key Cardiovascular Considerations
The potential for altered cholesterol is part of a wider set of cardiovascular factors to consider.
The therapy can, in some cases, lead to more serious cardiovascular effects or changes in heartbeat, such as a slow or fast pulse or pounding in the ears.
Other Potential Systemic Effects
Beyond the cardiovascular system, testosterone therapy can have other significant impacts.
These include risks like decreased sperm production and an increased risk of prostate cancer. There is also a list of rare but possible side effects, including urinary issues, dizziness, headaches, and testicular problems.
Common Pitfalls and Misconceptions
To use this therapy safely, it's crucial to understand the risks of improper use and to maintain a holistic view of your health rather than focusing on a single lab value.
The Danger of Misuse
Following your doctor's instructions precisely is non-negotiable.
Misusing testosterone patches or taking them without medical supervision can lead to serious cardiovascular or mental health consequences. The prescribed dose is tailored to your specific needs.
Focusing Solely on a Single Number
Viewing a change in cholesterol in isolation can be misleading.
Your doctor evaluates this number in the context of your overall health, the reasons you are on therapy, and other potential side effects. It is one piece of a much larger puzzle.
Making the Right Choice with Your Doctor
Your goal is to ensure the benefits of testosterone therapy outweigh the risks. This is an ongoing conversation and partnership with your healthcare provider.
- If your primary focus is managing potential side effects: Engage in regular blood tests and communicate openly with your physician about any new symptoms you experience.
- If your primary focus is understanding the overall risk: View cholesterol changes as one component of a comprehensive health assessment that also includes prostate, reproductive, and cardiovascular health.
- If you are concerned about a specific symptom: Report any side effect, such as blurred vision, urinary pain, or dizziness, to your doctor immediately for proper evaluation.
Ultimately, understanding the full scope of effects empowers you to partner effectively with your healthcare provider for a safe and successful treatment plan.
Summary Table:
| Potential Effect | Description | Key Consideration |
|---|---|---|
| Altered Lipid Profile | May change the balance of cholesterol and fats in the blood. | A known variable; monitored via routine blood tests. |
| Cardiovascular Risks | Includes potential for serious cardiovascular effects or changes in heartbeat. | Part of a broader risk-benefit assessment. |
| Other Systemic Effects | Can include decreased sperm production and increased risk of prostate cancer. | Requires comprehensive health monitoring beyond cholesterol. |
Partner with a Trusted Manufacturer for Your Transdermal Patch Needs
Navigating the complexities of hormone therapy requires reliable, high-quality products. Enokon is a bulk manufacturer of trusted transdermal patches and pain plasters for healthcare distributors and pharmaceutical brands.
Benefit from our technical expertise for custom R&D and product development, ensuring your therapies meet the highest standards of safety and efficacy.
Contact our experts today to discuss how we can support your product development and supply chain.
Visual Guide
Related Products
- Prostate Pain Kidney Health Care Patch for Men
- Far Infrared Heat Pain Relief Patches Transdermal Patches
- Medical Cooling Gel Patches for Fever Cooling Patches
- Menthol Gel Pain Relief Patch
- Icy Hot Menthol Medicine Pain Relief Patch
People Also Ask
- What serious side effects can transdermal estradiol cause? Understanding the Systemic Risks of Hormone Therapy
- How should the Ethinyl Estradiol; Norelgestromin patch be applied? A Guide to Correct Use & Maximum Effectiveness
- Is the Asenapine transdermal system safe to use during pregnancy? Understand the Risks and Benefits
- How can a parent ensure the Daytrana patch is working when the child wakes up? Apply it 2 hours before they rise.
- Why is a deaeration step critical during the production of high-quality transdermal films? Ensure Dosage Precision
- What is the titration schedule for methylphenidate transdermal? A Safe, Gradual Dosing Guide
- How soon can pregnancy occur after stopping the birth control patch? Fertility Returns Fast—Here’s What to Know
- What are the common side effects of the contraceptive patch? Know the signs to watch for.















