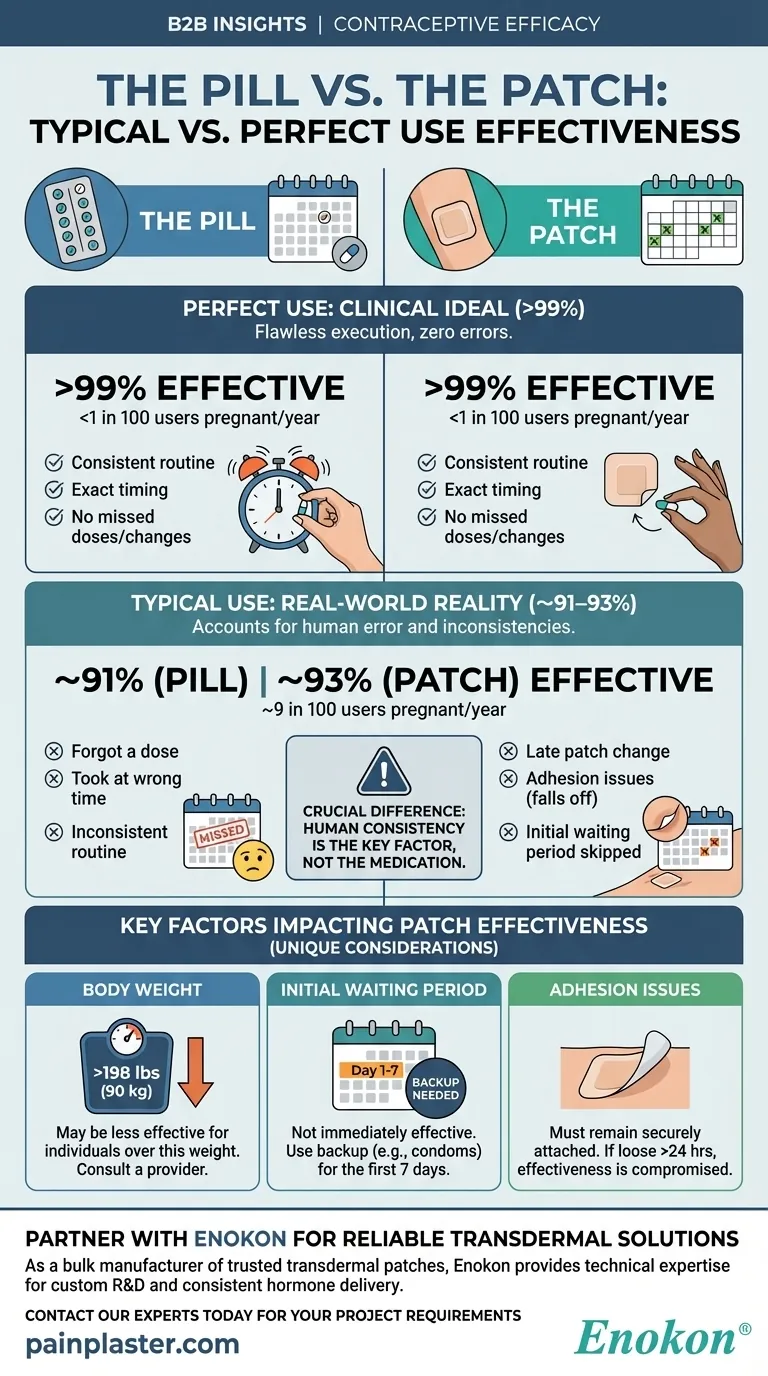
Here are the effectiveness rates for the pill and the patch. Both methods are over 99% effective at preventing pregnancy when used perfectly, meaning fewer than 1 in 100 users will become pregnant in a year. However, with typical, real-world use that accounts for human error, their effectiveness drops to about 91-93%, with roughly 9 in 100 users experiencing a pregnancy each year.
The crucial difference between 99% and 93% effectiveness for both the pill and the patch is not the method itself, but human consistency. The "typical use" rate reflects common, preventable mistakes like forgetting a dose or not changing a patch on time.

Defining the Gold Standard: "Perfect Use"
"Perfect use" is a clinical term that describes following the instructions for a contraceptive method without any errors, every single time. It represents the maximum potential effectiveness of the method under ideal conditions.
What Perfect Use Looks Like
For both the pill and the patch, perfect use means taking your dose or changing your patch at the exact prescribed time, without fail, for the entire cycle.
This requires a consistent routine and immediate correction of any mistakes according to the product's specific instructions.
The 99%+ Efficacy Rate
When used flawlessly, both methods are exceptionally effective. The continuous and correct delivery of hormones works as designed to prevent ovulation, making pregnancy extremely unlikely.
The Reality Check: "Typical Use"
"Typical use" reflects how people actually use contraception in their daily lives. This rate accounts for the mistakes, forgotten doses, and real-world scenarios that reduce a method's effectiveness.
Why Effectiveness Drops to 91-93%
The 8-percentage-point drop from perfect to typical use is almost entirely due to user error. This isn't a failure of the medication, but a reflection of normal human behavior.
Common issues include forgetting to take a pill, taking it at the wrong time, not changing a patch on the correct day, or a patch accidentally falling off without being replaced promptly.
The Cumulative Effect of Small Errors
A single mistake might not always lead to pregnancy, but inconsistent use over the course of a year significantly increases the statistical risk. The 9% failure rate accounts for the cumulative probability of these small errors resulting in an unintended pregnancy over 12 months.
Key Factors That Impact Patch Effectiveness
While the pill and patch have similar effectiveness rates, the patch has a few unique considerations you must be aware of. These factors can move you from the "perfect use" category to "typical use" without you realizing it.
Body Weight
The patch may be less effective for individuals who weigh more than 198 pounds (90 kg). It is critical to discuss this with your healthcare provider to determine if it is the right method for you.
Initial Waiting Period
The patch is not immediately effective. Unless you start using it within the first 5 days of your period, you must use a backup birth control method (like condoms) for the first 7 days to be protected.
Adhesion Issues
For the patch to work, it must remain securely attached to your skin. If the patch comes loose or falls off for more than 24 hours, its effectiveness is compromised, and backup contraception is required.
Making the Right Choice for Your Life
Understanding the difference between perfect and typical use is about choosing a method that aligns with your personal habits and lifestyle to ensure you stay as close to the "perfect use" rate as possible.
- If your primary focus is maximum protection: You must commit to a flawless routine, whether it's setting a daily alarm for the pill or a weekly calendar alert for the patch.
- If you know you're forgetful with daily tasks: The weekly patch may offer a more manageable schedule than a daily pill, reducing the number of opportunities for error.
- If you have specific health factors (like weighing over 198 lbs): You must consult a doctor, as the patch may not be your most effective hormonal option.
Ultimately, the most effective birth control method is the one you will use correctly and consistently.
Summary Table:
| Method | Perfect Use Effectiveness | Typical Use Effectiveness | Key Difference |
|---|---|---|---|
| The Pill | >99% (<1 in 100 users get pregnant/year) | ~91% (~9 in 100 users get pregnant/year) | Human error (forgetting a dose) |
| The Patch | >99% (<1 in 100 users get pregnant/year) | ~93% (~9 in 100 users get pregnant/year) | Human error (late patch change, adhesion issues) |
Need a reliable, high-quality transdermal patch for your brand or distribution network? As Enokon, a bulk manufacturer of trusted transdermal patches and pain plasters, we provide the technical expertise for custom R&D and development. Ensure your product delivers consistent, effective hormone delivery or pain relief for end-users. Contact our experts today to discuss your project requirements.
Visual Guide
Related Products
- Mugwort Wormwood Pain Relief Patch for Neck Pain
- Far Infrared Deep Heat Relief Patches Medicated Pain Relief Patches
- Cooling Fever Patches Color Change Cold Fever Patch
- Far Infrared Knee Pain Patch Heat Patches for Pain Relief
- Far Infrared Pain Patch Relief Pain Reliever for Back
People Also Ask
- What conditions contraindicate transdermal drug delivery? Key Risks & Safe Use Guidelines
- Why are ex vivo biological membranes used in diffusion experiments for transdermal drug delivery? Real-World Lab Insights
- What are common application site reactions with transdermal oxybutynin and how are they managed? Minimize Itch & Redness
- What ongoing care is required while using transdermal estradiol? Ensure Safe & Effective Hormone Therapy
- Function of High-Precision Dermatome in Transdermal Models: Standardizing Skin Thickness for Research Accuracy
- What is a nicotine patch and how does it work? A Guide to Quitting Smoking Successfully
- How should scopolamine patches be stored? Ensure Maximum Efficacy and Safety
- What is the key takeaway about the birth control patch? High Efficacy with Weekly Convenience