When using transdermal oxybutynin, the most common application site reactions are itchiness (pruritus) and redness (erythema). These reactions are typically mild to moderate and can be successfully managed with proactive skin care, primarily through consistent site rotation and the use of moisturizers.
The key to successful long-term use of the oxybutynin patch is not just reacting to skin irritation, but proactively preventing it. Simple, consistent skin care practices are the most effective tool for minimizing these common and generally mild side effects.

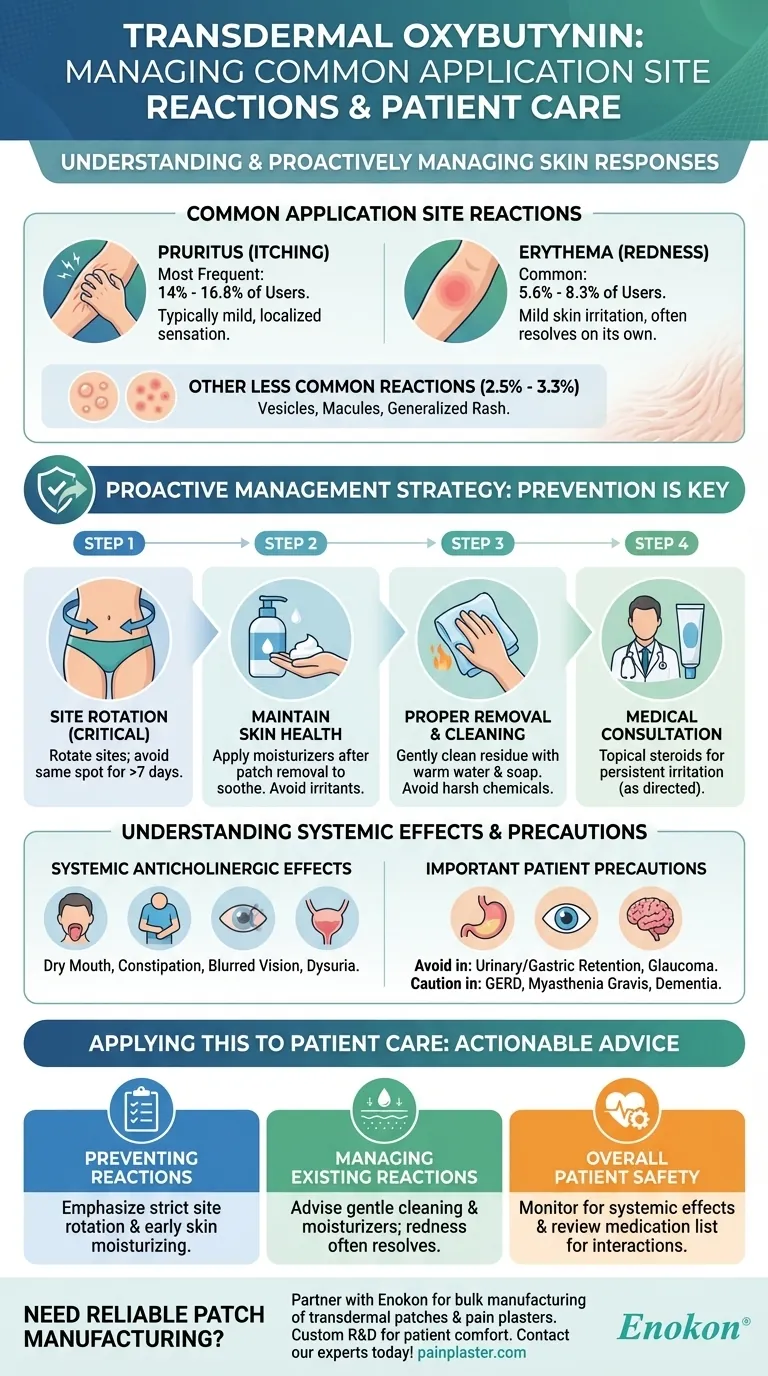
Identifying Common Application Site Reactions
Understanding what to expect is the first step in effective management. The skin's response to the patch is generally predictable and well-documented.
Pruritus (Itching)
Pruritus is the most frequently reported reaction, affecting 14% to 16.8% of users. This sensation is typically mild and localized to the area directly under and around the patch.
Erythema (Redness)
Localized redness at the application site is also common, occurring in 5.6% to 8.3% of users. This erythema is a sign of mild skin irritation and often resolves on its own after the patch is removed.
Other Less Common Reactions
In a smaller percentage of cases (2.5% to 3.3%), other reactions like vesicles (small blisters), macules (flat, red spots), or a more generalized rash may appear at the application site.
A Proactive Management Strategy
Effective management is centered on prevention. Counseling patients on a proper skin care routine can significantly reduce the incidence and severity of these reactions.
The Foundation: Site Rotation
The patch should be applied to the abdomen, hip, or buttock for 3-4 days. It is critical to rotate the application site with each new patch, avoiding the same spot for at least 7 days to allow the skin to fully recover.
Maintaining Skin Health
For mild itchiness, applying moisturizers to the area after the patch is removed can soothe the skin. Avoiding local irritants like harsh soaps or lotions on the application sites is also beneficial.
Proper Removal and Cleaning
Any adhesive residue left on the skin after removing the patch should be gently cleaned with warm water and soap. Avoid using alcohol or other harsh chemicals that can further irritate the skin.
When to Consider Topical Steroids
In cases of more persistent or bothersome irritation, a mild topical steroid can be used prudently as directed by a healthcare provider to calm the inflammation.
Understanding the Trade-offs and Systemic Effects
While local skin reactions are the most common issue, it's important to recognize that oxybutynin is absorbed into the body and can have other effects.
Beyond the Skin: Anticholinergic Side Effects
The transdermal system is designed to minimize systemic side effects, but they can still occur. These include dry mouth (xerostomia), constipation, blurred vision, and dysuria (painful urination).
Potential Drug Interactions
Oxybutynin can interact with other anticholinergic drugs, increasing the risk of side effects. It should also be used with caution alongside CNS depressants or any medication that can irritate the esophagus.
Important Patient Precautions
This treatment should be avoided in patients with conditions like urinary or gastric retention, uncontrolled narrow-angle glaucoma, and used cautiously in those with GERD, myasthenia gravis, or dementia.
How to Apply This to Patient Care
Translating this knowledge into clear, actionable advice is essential for ensuring patient compliance and treatment success.
- If your primary focus is preventing reactions: Emphasize a strict site rotation schedule and maintaining healthy, moisturized skin from the very first patch application.
- If your primary focus is managing existing mild reactions: Advise the use of gentle cleansers and moisturizers on the affected sites after patch removal, reassuring the patient that redness often resolves spontaneously.
- If your primary focus is overall patient safety: Be sure to monitor for systemic anticholinergic effects like dry mouth or confusion and always review the patient's full medication list for potential interactions.
By empowering patients with a clear understanding of these potential reactions and simple management techniques, you can help them achieve the full therapeutic benefit of transdermal oxybutynin.
Summary Table:
| Common Reaction | Frequency | Management Strategy |
|---|---|---|
| Pruritus (Itching) | 14% - 16.8% | Site rotation, moisturizers post-removal |
| Erythema (Redness) | 5.6% - 8.3% | Site rotation, gentle cleansing, resolves on its own |
| Other (Vesicles, Rash) | 2.5% - 3.3% | Consult healthcare provider; may require topical steroids |
Need a reliable transdermal patch manufacturer for your overactive bladder or pain management portfolio?
Partner with Enokon, a bulk manufacturer of reliable transdermal patches and pain plasters for healthcare and pharma distributors and brands. Benefit from our technical expertise for custom R&D and development, ensuring your products are designed with patient comfort and adherence in mind.
Contact our experts today to discuss your specific needs and how we can support your product development.
Visual Guide
Related Products
- Far Infrared Heat Pain Relief Patches Transdermal Patches
- Asthma Cough and Pain Relief Patch for Adults and Kids
- Heating Pain Relief Patches for Menstrual Cramps
- Far Infrared Deep Heat Relief Patches Medicated Pain Relief Patches
- Far Infrared Pain Patch Relief Pain Reliever for Back
People Also Ask
- What types of pain can the Deep Heat Pain Relief Back Patch be used for? Targeted Relief for Muscles & Joints
- How do Deep Heat Pain Relief Patches provide pain relief? Discover the Drug-Free Mechanism
- What are the common side effects of using the medicated heat patch? Understanding Risks & Safe Use
- How does capsaicin work in the medicated heat patch? The Science Behind Pain Relief
- What did the UK Million Women Study find regarding transdermal versus oral hormone therapy? A Safer Choice for Gallbladder Health















