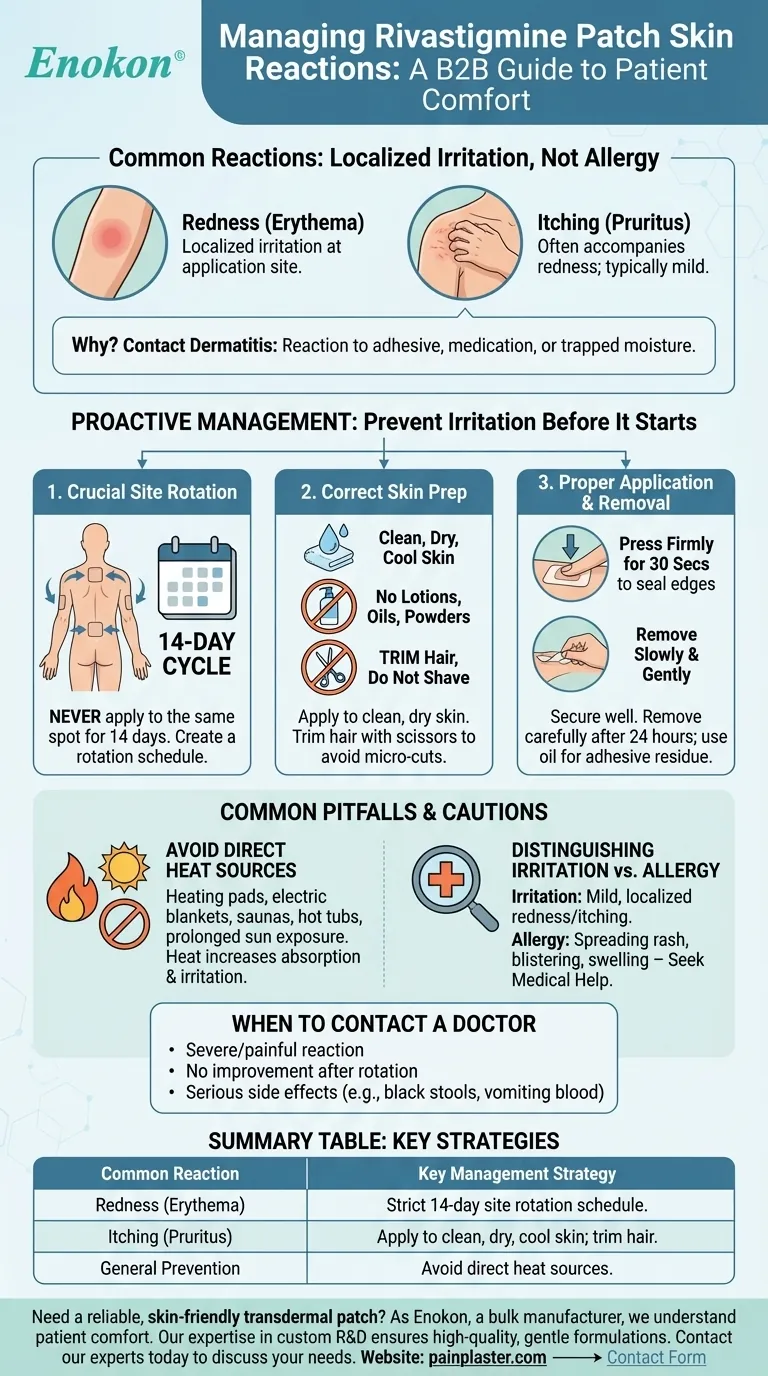
The most common skin reactions to the rivastigmine patch are redness (erythema) and itching (pruritus) at the application site. These symptoms are typically a form of localized skin irritation, not a systemic allergic reaction, and can often be prevented or minimized with a consistent and careful skin care routine.
The key to minimizing skin reactions from the rivastigmine patch is proactive management. By systematically rotating application sites and following proper skin preparation techniques, most irritation can be prevented before it starts.

Identifying Common Skin Reactions
Redness (Erythema)
The most frequently reported reaction is a patch of redness on the skin directly where the patch was applied. This is a sign of local irritation.
Itching (Pruritus)
Itching often accompanies the redness. While uncomfortable, it is usually mild and resolves after the patch is removed and the site is given time to recover.
Why These Reactions Occur
These reactions are typically a form of contact dermatitis. The skin is reacting to the adhesive, the medication itself, or the moisture trapped under the patch for 24 hours.
Proactive Management to Prevent Irritation
The Importance of Site Rotation
This is the single most critical step in preventing skin irritation. Never apply a new patch to the same exact spot for at least 14 days.
Create a rotation schedule for approved application sites, such as the upper or lower back, upper arms, or chest. This allows each area of skin to fully recover.
Preparing the Skin Correctly
Apply the patch to clean, dry, and cool skin that is free of any powders, oils, moisturizers, or lotions.
If there is hair, trim it with scissors rather than shaving. Shaving can create tiny cuts in the skin, increasing the risk of irritation.
Proper Application and Removal
Press the patch firmly in place for about 30 seconds to ensure the edges are sealed. Caregivers may find it helpful to write the date on the patch as a reminder.
After 24 hours, remove the patch slowly and gently to avoid damaging fragile skin. If any adhesive remains, you can clean it off with an oil-based substance like olive oil.
Common Pitfalls and Cautions
Avoid Direct Heat Sources
You must avoid placing external heat sources over the patch. This includes heating pads, electric blankets, saunas, hot tubs, and heated water beds.
Prolonged exposure to direct sunlight on the patch area should also be avoided. Heat can cause the medication to be absorbed too quickly and can worsen skin irritation.
Distinguishing Irritation from Allergy
Mild, localized redness and itching that resolves is considered irritation.
A more severe reaction, such as a rash that spreads, blistering, or intense swelling, may indicate a true allergy. This requires immediate medical consultation.
When to Contact Your Doctor
You should always contact a healthcare provider if a skin reaction is severe, painful, or does not improve after you stop applying patches to that area.
It is critical to seek immediate medical help for any serious side effects, such as black or bloody stools, vomiting blood, seizures, or painful urination, as these are unrelated to skin irritation and indicate a more serious issue.
Making the Right Choice for Your Goal
- If your primary focus is prevention: Establish a strict 14-day site rotation schedule from the very first day of treatment.
- If your primary focus is managing mild irritation: Double-check that you are trimming (not shaving) hair and applying the patch to completely clean, dry, and un-moisturized skin.
- If your primary focus is addressing a persistent reaction: Stop applying patches to that area and consult your doctor for guidance, which may include antihistamines or topical treatments.
By implementing these careful and consistent practices, you can effectively manage the rivastigmine patch as a safe and comfortable part of the treatment plan.
Summary Table:
| Common Reaction | Key Management Strategy |
|---|---|
| Redness (Erythema) | Strict 14-day site rotation schedule. |
| Itching (Pruritus) | Apply to clean, dry, cool skin; trim hair, don't shave. |
| General Prevention | Avoid direct heat sources on the patch area. |
Need a reliable, skin-friendly transdermal patch? As Enokon, a bulk manufacturer of reliable transdermal patches and pain plasters for healthcare/pharma distributors and brands, we understand the importance of patient comfort and adherence. Our technical expertise in custom R&D and development ensures high-quality, gentle formulations. Let us help you create a superior product. Contact our experts today to discuss your needs.
Visual Guide
Related Products
- Herbal Eye Protection Patch Eye Patch
- Far Infrared Deep Heat Relief Patches Medicated Pain Relief Patches
- Asthma Cough and Pain Relief Patch for Adults and Kids
- Menthol Gel Pain Relief Patch
- Icy Hot Menthol Medicine Pain Relief Patch
People Also Ask
- What are the steps for properly using eye patches? Maximize Benefits for Your Delicate Eye Area
- Should under eye patches be applied before or after moisturizer? Optimize Your Skincare Routine
- What factors should be considered when purchasing eye patches? Essential Guide for Safe & Effective Use
- What are the main benefits of using eye patches in a skincare routine? Revitalize Your Under-Eye Area
- How quickly can you see results from using under eye patches? Instant Brightening & Long-Term Benefits
















