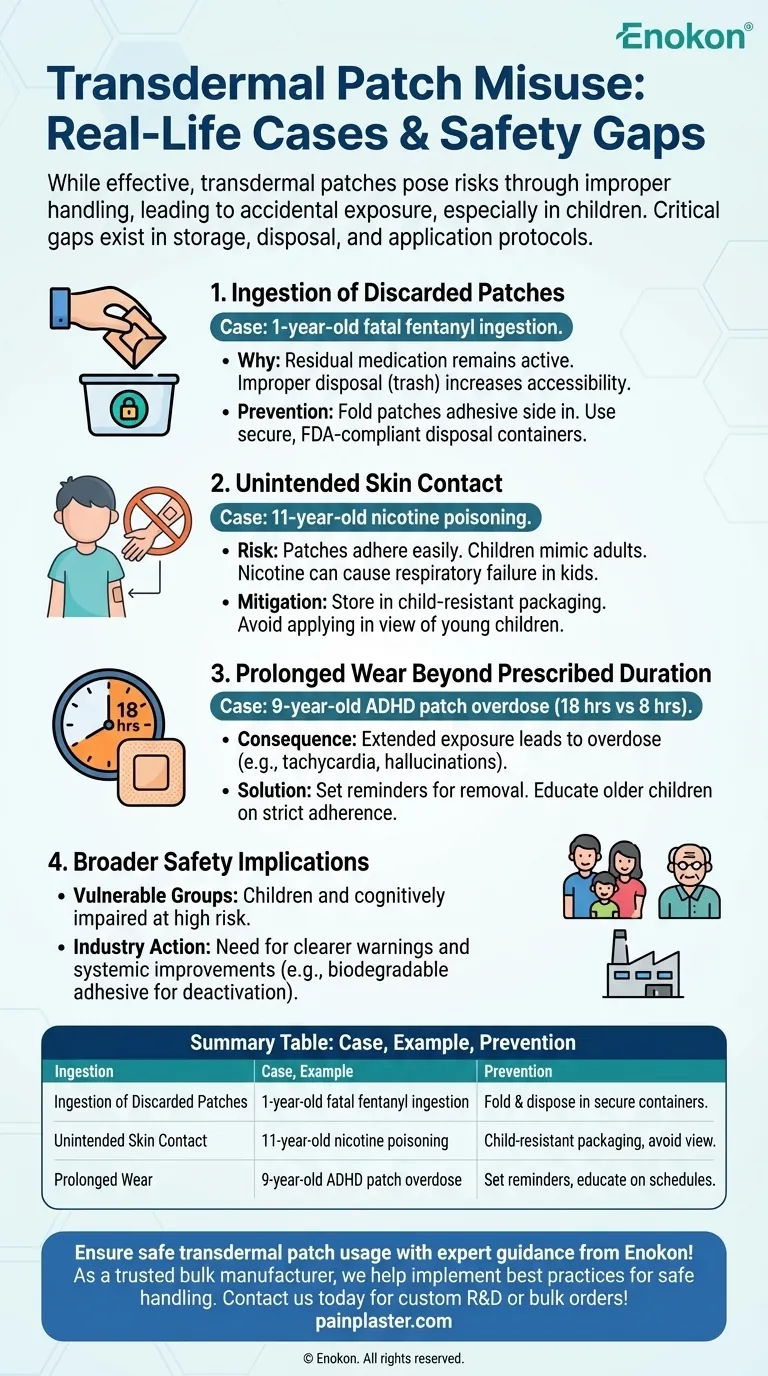
Transdermal patches, while effective for controlled drug delivery, have been associated with misuse cases, often involving accidental exposure or improper use, particularly among children. These incidents highlight critical safety gaps in storage, disposal, and application protocols. For example, ingestion of discarded patches, unintended skin contact, or prolonged wear beyond prescribed durations can lead to severe poisoning or adverse neurological effects. Such cases underscore the need for stricter handling guidelines and public awareness to prevent harm, especially in households with vulnerable individuals.

Key Points Explained:
-
Ingestion of Discarded Patches
- A 1-year-old died after finding and ingesting a used transdermal patch containing fentanyl, a potent opioid.
- Why it happens: Residual medication remains active in patches even after use. Improper disposal (e.g., tossing in trash) increases accessibility to children or pets.
- Prevention: Patches should be folded (adhesive side in) and disposed of in secure containers, following FDA guidelines for opioid patches.
-
Unintended Skin Contact
- An 11-year-old developed nicotine poisoning after applying his mother’s nicotine replacement patch.
- Risk factors: Patches adhere easily to skin, and children may mimic adult behavior. Nicotine patches can cause nausea, seizures, or even respiratory failure in pediatric cases.
- Mitigation: Store patches in child-resistant packaging and avoid applying them in view of young children.
-
Prolonged Wear Beyond Prescribed Duration
- A 9-year-old experienced agitation and confusion after wearing a methylphenidate (ADHD medication) patch for 18 hours instead of the prescribed 8.
- Consequence: Extended exposure can lead to overdose symptoms, including tachycardia or hallucinations, due to sustained drug release.
- Solution: Caregivers must set reminders to remove patches on time and educate older children about strict adherence to wear schedules.
-
Broader Safety Implications
- Vulnerable groups: Children and cognitively impaired individuals are at higher risk due to curiosity or inability to recognize hazards.
- Industry action: Some manufacturers now include clearer warnings and disposal instructions, but systemic improvements (e.g., biodegradable adhesive to deactivate drugs post-use) are needed.
These cases reveal how everyday healthcare tools, like transdermal patches, require vigilant handling to balance therapeutic benefits with safety. Could your storage habits be unknowingly putting others at risk? Simple steps—like locking patches away and using disposal kits—can prevent tragedies.
Summary Table:
| Case | Example Incident | Prevention Tips |
|---|---|---|
| Ingestion of Discarded Patches | 1-year-old died after ingesting a used fentanyl patch. | Fold patches (adhesive side in) and dispose in secure containers. |
| Unintended Skin Contact | 11-year-old developed nicotine poisoning from a nicotine patch. | Store patches in child-resistant packaging; avoid applying in view of children. |
| Prolonged Wear | 9-year-old experienced agitation after wearing an ADHD patch for 18 hours. | Set reminders to remove patches on time; educate children on wear schedules. |
Ensure safe transdermal patch usage with expert guidance from Enokon!
As a trusted bulk manufacturer of reliable transdermal patches and pain plasters, we help healthcare distributors and brands implement best practices for safe handling, storage, and disposal. Our technical expertise ensures your products meet the highest safety standards while delivering effective therapeutic results.
Contact us today to discuss custom R&D solutions or bulk orders tailored to your needs!
Visual Guide
Related Products
- Far Infrared Heat Pain Relief Patches Transdermal Patches
- Herbal Eye Protection Patch Eye Patch
- Heating Pain Relief Patches for Menstrual Cramps
- Menthol Gel Pain Relief Patch
- Icy Hot Menthol Medicine Pain Relief Patch
People Also Ask
- What types of pain can the Deep Heat Pain Relief Back Patch be used for? Targeted Relief for Muscles & Joints
- What did the UK Million Women Study find regarding transdermal versus oral hormone therapy? A Safer Choice for Gallbladder Health
- How does capsaicin work in the medicated heat patch? The Science Behind Pain Relief
- What are the common side effects of using the medicated heat patch? Understanding Risks & Safe Use
- What are the key features of the Deep Heat Pain Relief Back Patch? Get Up to 16 Hours of Drug-Free Relief

















