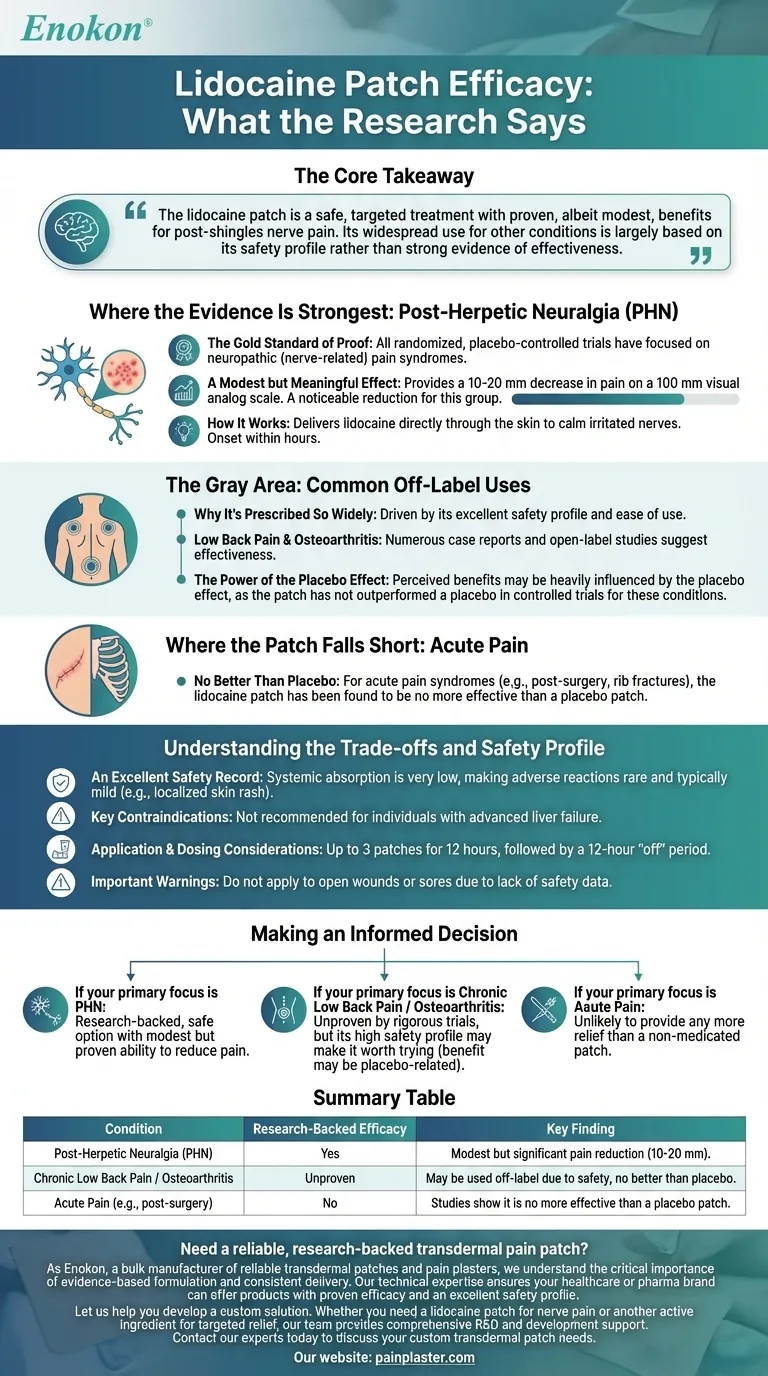
Based on controlled research, the 5% lidocaine patch has modest but significant efficacy for one specific condition: post-herpetic neuralgia (PHN), the nerve pain that can linger after a shingles infection. For most other types of pain, including acute pain from surgery or injuries, rigorous studies have found it is no more effective than a placebo.
The core takeaway from clinical research is that the lidocaine patch is a safe, targeted treatment with proven, albeit modest, benefits for post-shingles nerve pain. Its widespread use for other conditions is largely based on its safety profile rather than strong evidence of effectiveness.

Where the Evidence Is Strongest: Post-Herpetic Neuralgia
The Gold Standard of Proof
All randomized, placebo-controlled trials—the most reliable form of medical research—have focused on neuropathic (nerve-related) pain syndromes.
A Modest but Meaningful Effect
In patients with PHN, the patch provides a 10-20 mm decrease in pain on a 100 mm visual analog scale. This represents a noticeable, though not complete, reduction in pain for this specific group.
How It Works
The patch delivers lidocaine directly through the skin to the painful area, calming irritated nerves. The onset of this analgesic effect typically occurs within a few hours of application.
The Gray Area: Common Off-Label Uses
Why It's Prescribed So Widely
Despite limited proven efficacy beyond PHN, the patch is frequently used "off-label" for other conditions. This is primarily driven by its excellent safety profile and ease of use compared to oral pain medications.
Low Back Pain and Osteoarthritis
Numerous case reports and open-label studies suggest the patch may be effective for chronic low back pain, osteoarthritis, and other neuropathic conditions.
The Power of the Placebo Effect
It is crucial to interpret these non-controlled reports with caution. Researchers note that the perceived benefits in these cases may be heavily influenced by the placebo effect, as the patch has not outperformed a placebo in controlled trials for these conditions.
Where the Patch Falls Short: Acute Pain
No Better Than Placebo
For acute pain syndromes, such as pain following surgery or from rib fractures, controlled studies are clear. The lidocaine patch has been found to be no more effective than a placebo patch.
Understanding the Trade-offs and Safety Profile
An Excellent Safety Record
Systemic absorption of lidocaine from the patch is very low, making adverse reactions rare and typically mild. The most common side effect is a localized, non-serious skin rash or irritation.
Key Contraindications
The patch is not recommended for individuals with advanced liver failure, as their body cannot clear the lidocaine effectively.
Application and Dosing Considerations
Standard dosing is up to three patches worn for 12 hours, followed by a 12-hour "off" period. Some patients report that their pain worsens during this off period.
Important Warnings on Use
The manufacturer warns against applying the patch to open wounds or sores due to a lack of safety data for this type of application.
Making an Informed Decision
Understanding the evidence allows you to work with your clinician to set realistic expectations.
- If your primary focus is treating nerve pain after a shingles infection (PHN): The lidocaine patch is a research-backed, safe option with a modest but proven ability to reduce your pain.
- If your primary focus is chronic low back pain or osteoarthritis: Its effectiveness is unproven by rigorous trials, but its high safety profile may make it worth trying, keeping in mind that any benefit may be related to a placebo response.
- If your primary focus is acute pain from an injury or surgery: Current evidence strongly suggests the lidocaine patch is unlikely to provide any more relief than a non-medicated patch.
Knowing where the lidocaine patch is effective—and where it is not—empowers you to make the best decision for managing your specific type of pain.
Summary Table:
| Condition | Research-Backed Efficacy | Key Finding |
|---|---|---|
| Post-Herpetic Neuralgia (PHN) | Yes | Modest but significant pain reduction (10-20 mm on a 100 mm scale). |
| Chronic Low Back Pain / Osteoarthritis | Unproven | May be used off-label due to safety, but no better than placebo in controlled trials. |
| Acute Pain (e.g., post-surgery) | No | Studies show it is no more effective than a placebo patch. |
Need a reliable, research-backed transdermal pain patch?
As Enokon, a bulk manufacturer of reliable transdermal patches and pain plasters, we understand the critical importance of evidence-based formulation and consistent delivery. Our technical expertise ensures your healthcare or pharma brand can offer products with proven efficacy and an excellent safety profile.
Let us help you develop a custom solution. Whether you need a lidocaine patch for nerve pain or another active ingredient for targeted relief, our team provides comprehensive R&D and development support.
Contact our experts today to discuss your custom transdermal patch needs.
Visual Guide
Related Products
- Lidocaine Hydrogel Pain Relief Patch for Pain Relief
- Asthma Cough and Pain Relief Patch for Adults and Kids
- Prostate Pain Kidney Health Care Patch for Men
- Far Infrared Deep Heat Relief Patches Medicated Pain Relief Patches
- Icy Hot Menthol Medicine Pain Relief Patch
People Also Ask
- What were the median pain scores before and after the use of the lidocaine plaster? See the Data-Backed Relief
- Who should avoid using lidocaine patches? Key Safety Considerations for Pain Relief
- What was the objective of the study on the lidocaine patch 5%? Evaluating Pain Quality & Safety as Add-On Therapy
- Why is Polyethylene Terephthalate (PET) film typically selected as the release liner for lidocaine transdermal patches?
- Is there strong evidence supporting the effectiveness of lidocaine patches for back pain? The Scientific Verdict
- What information should be shared with healthcare providers before using lidocaine plasters? Ensure Safe Pain Relief
- What are lidocaine patches used for? Targeted Relief for Nerve & Muscle Pain
- How quickly do lidocaine patches take effect? Fast & Long-Lasting Pain Relief Explained