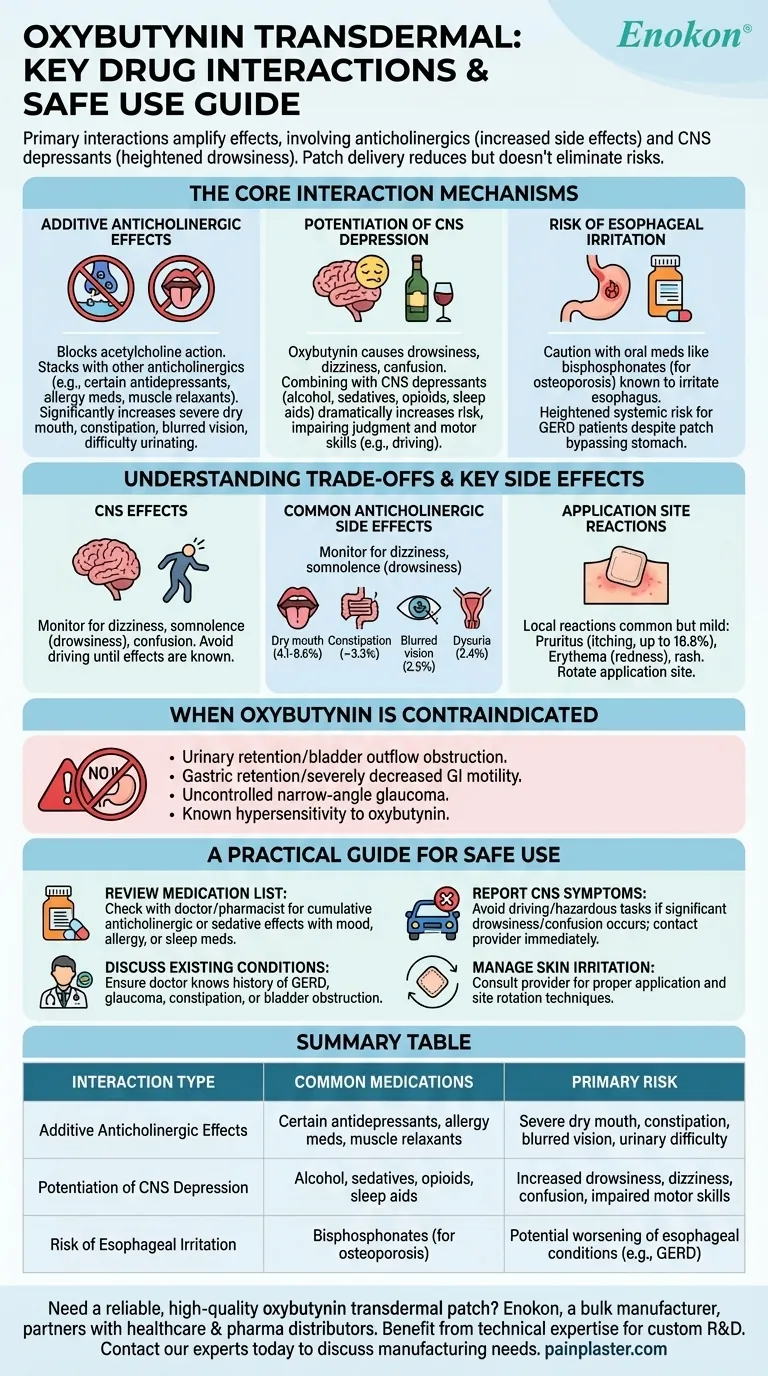
The primary drug interactions associated with oxybutynin transdermal involve medications that amplify its core effects. This includes other anticholinergic drugs, which increase side effects like dry mouth and constipation, and central nervous system (CNS) depressants, which heighten drowsiness and dizziness. Caution is also advised when it is used with medications known to irritate the esophagus.
While the transdermal patch delivery system can reduce some side effects compared to oral tablets, it does not eliminate the risk of drug interactions. The central challenge is managing the cumulative impact of medications that share similar side effect profiles.

The Core Interaction Mechanisms
To use oxybutynin safely, it's essential to understand why these interactions occur. The risks stem from additive effects, where two different drugs create a combined impact greater than either one alone.
Additive Anticholinergic Effects
Oxybutynin works by blocking the action of a neurotransmitter called acetylcholine. Many other common medications—including certain antidepressants, allergy medications, and muscle relaxants—also have this anticholinergic effect.
When taken together, their effects stack, significantly increasing the likelihood and severity of side effects such as severe dry mouth, constipation, blurred vision, and difficulty urinating.
Potentiation of CNS Depression
Oxybutynin itself can cause drowsiness, dizziness, confusion, and even hallucinations. These are known as central nervous system (CNS) effects.
Combining it with other CNS depressants like alcohol, sedatives, opioids, or sleep aids dramatically increases this risk. This can impair judgment and motor skills, making activities like driving or operating heavy machinery dangerous.
Risk of Esophageal Irritation
Certain oral medications, such as bisphosphonates used for osteoporosis, are known to cause or worsen irritation of the esophagus (esophagitis).
While the transdermal patch bypasses the stomach, caution is still advised when using it alongside these drugs, as there may still be a heightened systemic risk for patients with conditions like GERD.
Understanding the Trade-offs and Key Side Effects
Knowing the potential interactions is only half the battle. You must also be able to recognize the resulting symptoms, which range from mild annoyances to serious safety concerns.
Central Nervous System (CNS) Effects
Patients must be monitored for signs of cognitive impact. Be aware of any new or worsening dizziness, somnolence (drowsiness), or confusion.
Because of these potential effects, you should avoid driving until you know how the medication affects you.
Common Anticholinergic Side Effects
The most frequently reported side effects are directly related to oxybutynin's primary mechanism. These include:
- Dry mouth (xerostomia), reported in 4.1% to 9.6% of users.
- Constipation, affecting around 3.3% of users.
- Blurred vision (2.5%) and dysuria, or painful urination (2.4%).
Application Site Reactions
Because the drug is delivered through the skin, local reactions are common but usually mild.
These include pruritus (itching), which is the most common side effect overall (up to 16.8%), along with erythema (redness), rash, or small vesicles at the patch site. Rotating the application site regularly helps minimize this irritation.
When Oxybutynin is Contraindicated
This medication is not safe for everyone. It is strictly contraindicated (should not be used) in patients with:
- Urinary retention or bladder outflow obstruction
- Gastric retention or severely decreased gastrointestinal motility
- Uncontrolled narrow-angle glaucoma
- Known hypersensitivity to oxybutynin
A Practical Guide for Safe Use
Your goal is to get the benefits of the medication while minimizing risk. This is achieved through awareness and clear communication with your healthcare team.
- If you take medications for mood, allergies, or sleep: Review your full medication list with your doctor or pharmacist to identify any potential for cumulative anticholinergic or sedative effects.
- If you have existing GI or urinary conditions: Ensure your doctor is fully aware of your history with GERD, glaucoma, constipation, or bladder obstruction before you begin treatment.
- If you experience significant drowsiness or confusion: Do not drive or perform hazardous tasks, and report the symptom to your provider immediately, as a dose adjustment or change may be needed.
- If you develop persistent skin irritation: Speak to your provider about proper application techniques and site rotation to manage local side effects.
Proactive communication with your healthcare provider is the most effective strategy for using oxybutynin transdermal safely and effectively.
Summary Table:
| Interaction Type | Common Medications | Primary Risk |
|---|---|---|
| Additive Anticholinergic Effects | Certain antidepressants, allergy meds, muscle relaxants | Severe dry mouth, constipation, blurred vision, urinary difficulty |
| Potentiation of CNS Depression | Alcohol, sedatives, opioids, sleep aids | Increased drowsiness, dizziness, confusion, impaired motor skills |
| Risk of Esophageal Irritation | Bisphosphonates (for osteoporosis) | Potential worsening of esophageal conditions (e.g., GERD) |
Need a reliable, high-quality oxybutynin transdermal patch?
As Enokon, a bulk manufacturer of trusted transdermal patches and pain plasters, we partner with healthcare and pharma distributors and brands. Benefit from our technical expertise for custom R&D and development to ensure your products meet the highest standards of safety and efficacy.
Contact our experts today to discuss your manufacturing needs.
Visual Guide
Related Products
- Far Infrared Heat Pain Relief Patches Transdermal Patches
- Far Infrared Deep Heat Relief Patches Medicated Pain Relief Patches
- Asthma Cough and Pain Relief Patch for Adults and Kids
- Heating Pain Relief Patches for Menstrual Cramps
- Capsaicin Chili Medicated Pain Relief Patches
People Also Ask
- What did the UK Million Women Study find regarding transdermal versus oral hormone therapy? A Safer Choice for Gallbladder Health
- How does capsaicin work in the medicated heat patch? The Science Behind Pain Relief
- Can heat patches be used for fresh injuries? Avoid This Common Mistake for Faster Recovery
- What are the key features of the Deep Heat Pain Relief Back Patch? Get Up to 16 Hours of Drug-Free Relief
- What are the common side effects of using the medicated heat patch? Understanding Risks & Safe Use

















