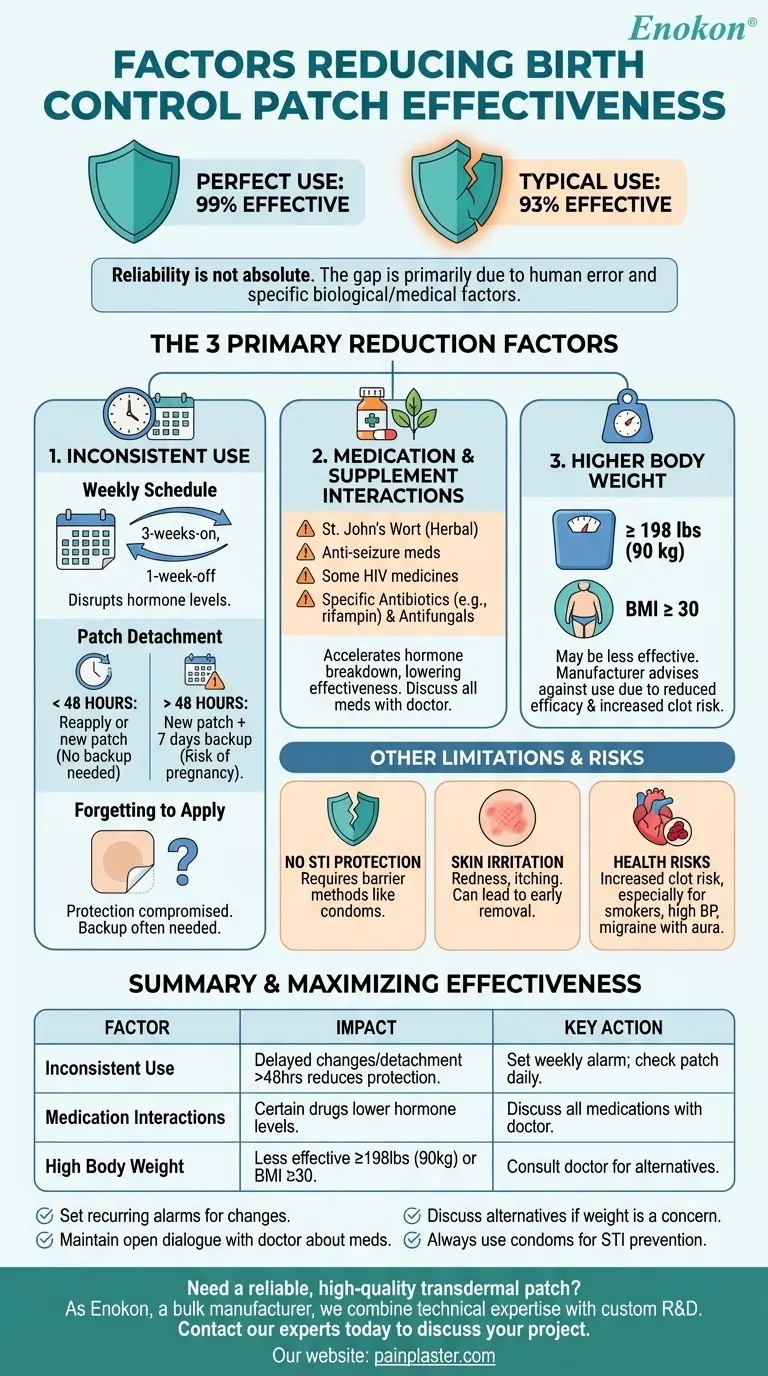
The birth control patch is highly effective, but its reliability is not absolute. Its effectiveness can be significantly reduced by three primary factors: inconsistent or incorrect use, interactions with certain medications and supplements, and higher body weight. Forgetting to change the patch on schedule or having it fall off for an extended period are the most common reasons for failure.
The difference between the patch's 99% effectiveness with perfect use and its 93% effectiveness with typical use is almost entirely explained by human error and specific biological or medical factors. Understanding these variables is critical to relying on it safely.

The Critical Role of Consistent Use
The most significant factor reducing the patch's effectiveness is how it's used in the real world. The gap between "perfect use" and "typical use" comes down to small, preventable mistakes.
The Weekly Change Schedule
The patch is designed to be changed once a week on the same day for three consecutive weeks, followed by one patch-free week. Deviating from this schedule can disrupt the consistent hormone levels needed to prevent ovulation.
If a Patch Falls Off
The patch's adhesive is strong, but it can detach. If it has been off for less than 48 hours (2 days), you can reapply it or apply a new one immediately without needing backup contraception.
If the patch has been detached for more than 48 hours, you are no longer protected against pregnancy. You should apply a new patch immediately, start a new "patch change day," and use a backup method of birth control (like condoms) for the next seven days.
Forgetting to Apply a New Patch
If you forget to apply a new patch at the start of a cycle or are late changing it during your cycle, your protection may be compromised. The specific steps to take depend on how long you have delayed, but in most cases, you will need to use backup contraception for at least one week.
External Factors That Interfere with Effectiveness
Even with perfect use, certain external and biological factors can interfere with the patch's ability to deliver a sufficient dose of hormones.
Medication and Supplement Interactions
Several medications can accelerate the breakdown of hormones from the patch, making it less effective. It is crucial to discuss all medications with your doctor.
Key culprits include:
- The herbal supplement St. John's Wort
- Certain anti-seizure medications
- Some HIV medicines
- Specific antibiotics (like rifampin) and antifungals
The Impact of Body Weight
The patch has been shown to be less effective in women who weigh 198 pounds (90 kg) or more. The manufacturer also advises against its use in individuals with a Body Mass Index (BMI) of 30 or greater due to both reduced effectiveness and an increased risk of blood clots.
Understanding the Trade-offs and Limitations
To use the patch effectively, you must understand its inherent limitations beyond just preventing pregnancy.
No Protection Against STIs
The birth control patch releases hormones to prevent pregnancy; it provides zero protection against sexually transmitted infections (STIs) like HIV, chlamydia, or herpes. Barrier methods like condoms are still necessary for STI prevention.
Potential for Skin Irritation
Some users experience redness, itching, or irritation at the application site. While often minor, this can be a significant disadvantage and may tempt a user to remove the patch early, compromising its effectiveness.
Increased Health Risks for Some
The patch, like many hormonal contraceptives, can increase the risk of blood clots, particularly in individuals who smoke, have unmanaged high blood pressure, or have a history of migraines with aura. It is not a suitable option for everyone.
How to Maximize the Patch's Effectiveness
Choosing and using contraception is about matching the method to your body and lifestyle.
- If your primary focus is preventing pregnancy: Set a recurring weekly alarm for patch changes and always check that the patch is firmly in place each day.
- If you take any other medications or supplements: Maintain an open dialogue with your doctor to ensure nothing you take will interfere with the patch's hormones.
- If you weigh 198 pounds (90 kg) or more: Discuss alternative contraceptive methods with your healthcare provider, as the patch may not be the most reliable option for you.
- If you are concerned about STIs: Always use a barrier method like condoms in addition to the patch, as it offers no protection against sexually transmitted infections.
By understanding these factors, you can use the birth control patch with confidence and control.
Summary Table:
| Factor | Impact on Effectiveness | Key Action |
|---|---|---|
| Inconsistent Use | Delayed patch changes or detachment for >48 hours reduces protection. | Set a weekly alarm; check patch daily. |
| Medication Interactions | Certain drugs (e.g., St. John's Wort, some antibiotics) can lower hormone levels. | Discuss all medications with your doctor. |
| High Body Weight | Less effective for individuals weighing 198 lbs (90 kg) or with a BMI ≥30. | Consult a doctor for alternative options. |
Need a reliable, high-quality transdermal patch? As Enokon, a bulk manufacturer of trusted transdermal patches and pain plasters for healthcare and pharmaceutical distributors, we combine technical expertise with custom R&D to deliver products you can count on. Let us help you develop a solution that meets your specific needs. Contact our experts today to discuss your project.
Visual Guide
Related Products
- Heating Pain Relief Patches for Menstrual Cramps
- Far Infrared Deep Heat Relief Patches Medicated Pain Relief Patches
- Asthma Cough and Pain Relief Patch for Adults and Kids
- Far Infrared Pain Patch Relief Pain Reliever for Back
- Capsaicin Chili Medicated Pain Relief Patches
People Also Ask
- Can heating pads be used with pain patches? Risks & Safety Tips
- How do Deep Heat Pain Relief Patches provide pain relief? Discover the Drug-Free Mechanism
- What are the key features of the Deep Heat Pain Relief Back Patch? Get Up to 16 Hours of Drug-Free Relief
- Why should heating pads not be used with transdermal patches? Avoid Overdose & Skin Risks
- How does the Deep Heat Back Patch work? A Drug-Free Solution for Targeted Pain Relief














