For safe transdermal fentanyl use, the essential interprofessional strategies are coordinated patient monitoring, proactive screening for misuse, unified communication among all team members, and comprehensive patient education. This system ensures every professional contributes to a shared safety net, from prescribing to administration and follow-up.
The core principle of transdermal fentanyl safety is not the responsibility of a single practitioner, but the result of a deliberate, multi-disciplinary system. Each professional—clinician, pharmacist, and nurse—must execute their specific role while maintaining constant communication to protect the patient from the inherent risks of this potent opioid.

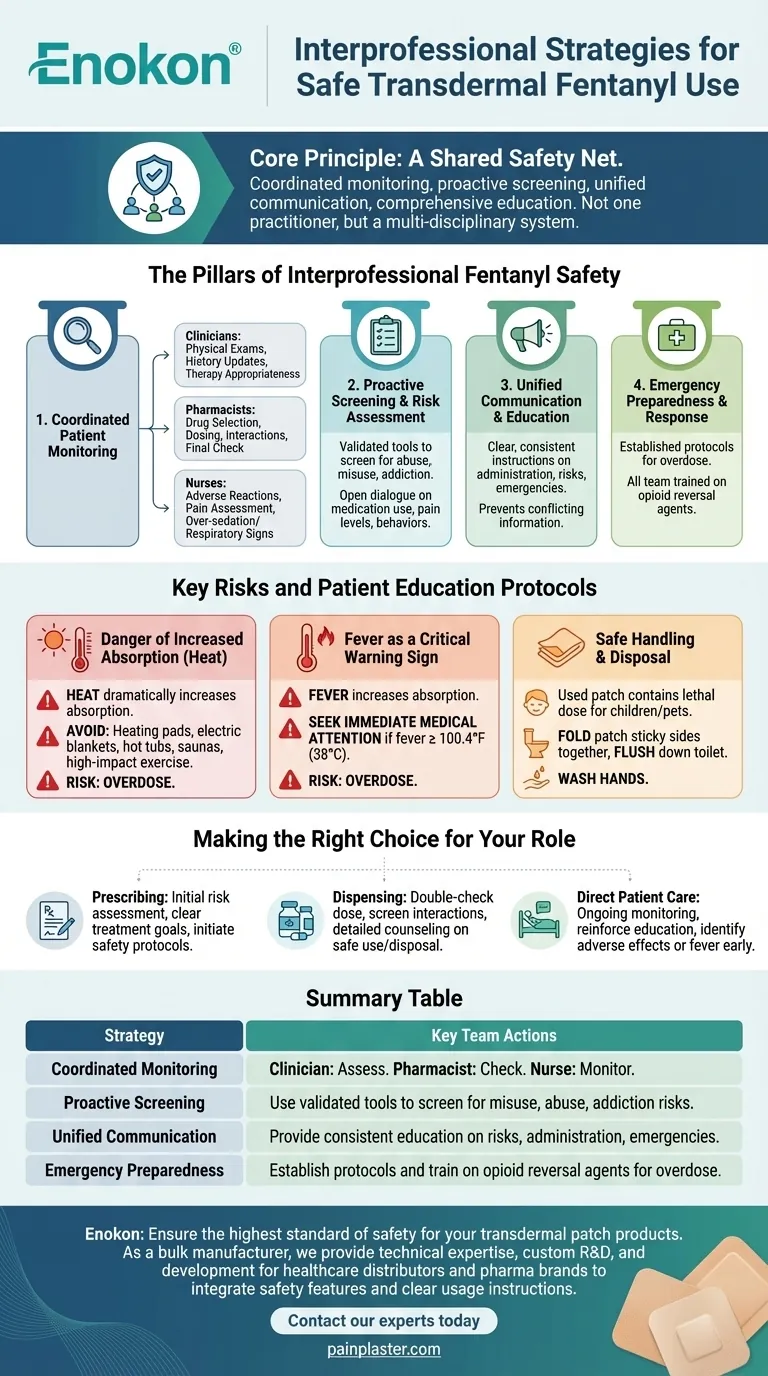
The Pillars of Interprofessional Fentanyl Safety
Transdermal fentanyl is a powerful tool for managing severe chronic pain, but its potency demands a highly structured safety approach. Effective collaboration is the only way to mitigate its significant risks.
H3: Coordinated Patient Monitoring
Continuous, multi-faceted monitoring is the foundation of patient safety. Each professional has a distinct but overlapping responsibility.
Clinicians are responsible for conducting initial and ongoing physical exams and medical history updates to ensure the continued appropriateness of the therapy.
Pharmacists provide critical consultations on drug selection, dosing, and potential interactions, acting as a final safety check before the medication reaches the patient.
Nurses are on the front line, monitoring for adverse reactions, assessing pain levels, and watching for early signs of over-sedation or respiratory depression.
H3: Proactive Screening and Risk Assessment
A key team function is to screen for potential abuse, misuse, and the development of addiction or physical dependence.
This involves using validated screening tools and maintaining an open dialogue with the patient about their medication use, pain levels, and any concerning behaviors. Recognizing these issues early is a shared responsibility.
H3: Unified Communication and Education
Clear and consistent communication is vital, both among team members and with the patient and their family.
The healthcare team must provide clear, unified instructions on proper administration, risks, and emergency procedures. This prevents conflicting information and empowers the patient to be an active participant in their own safety.
H3: Emergency Preparedness and Response
Every member of the healthcare team must be prepared for a worst-case scenario.
This requires having established emergency protocols for life-threatening conditions like overdose. All team members should be trained in the use of opioid reversal agents and know their role in an emergency.
Key Risks and Patient Education Protocols
A major part of the team's responsibility is educating the patient on critical safety measures. These are not suggestions but essential rules for preventing a therapeutic dose from becoming a dangerous one.
H3: The Danger of Increased Absorption
Patients must understand that heat dramatically increases the rate at which fentanyl is absorbed through the skin, which can easily lead to an overdose.
The team must explicitly warn patients to avoid all external heat sources near the patch, including heating pads, electric blankets, hot tubs, and saunas. High-impact exercise or anything that significantly raises body temperature should also be avoided.
H3: Fever as a Critical Warning Sign
A fever can also increase fentanyl absorption and is a medical emergency for a patient using the patch.
The team must instruct the patient to seek immediate medical attention for a fever of 100.4°F (38°C) or higher.
H3: Safe Handling and Disposal
The risk of fentanyl exposure extends beyond the patient. Even a used patch contains enough medication to be lethal to a child or pet.
Patients must be taught to fold the used patch in half with the sticky sides together and immediately flush it down a toilet. They must also wash their hands with soap and water after handling any patch.
Making the Right Choice for Your Role
A successful safety program depends on each professional understanding their specific contribution to the collective goal.
- If your primary focus is prescribing: Your key responsibility is the initial risk assessment, setting clear treatment goals, and initiating the conversation about safety protocols.
- If your primary focus is dispensing: Your role is crucial for double-checking the dose, screening for drug interactions, and providing the first wave of detailed patient counseling on safe use and disposal.
- If your primary focus is direct patient care: You are essential for ongoing monitoring, reinforcing education at every encounter, and being the first to identify adverse effects or signs of fever.
Ultimately, a coordinated and vigilant interprofessional team is the most effective safeguard for patients using transdermal fentanyl.
Summary Table:
| Strategy | Key Team Actions |
|---|---|
| Coordinated Monitoring | Clinician: Assess therapy appropriateness. Pharmacist: Check dose/interactions. Nurse: Monitor for adverse effects. |
| Proactive Screening | Team uses validated tools to screen for misuse, abuse, and addiction risks. |
| Unified Communication | All members provide consistent patient education on risks, administration, and emergencies. |
| Emergency Preparedness | Team establishes protocols and trains on the use of opioid reversal agents for overdose. |
Ensure the highest standard of safety for your transdermal patch products. As Enokon, a bulk manufacturer of reliable transdermal patches and pain plasters, we provide more than just manufacturing. Our technical expertise supports healthcare distributors and pharma brands with custom R&D and development, helping you integrate critical safety features and clear usage instructions directly into your product design. Let's collaborate to create safer, more effective transdermal solutions for patients.
Contact our experts today to discuss your specific needs.
Visual Guide
Related Products
- Far Infrared Deep Heat Relief Patches Medicated Pain Relief Patches
- Menthol Gel Pain Relief Patch
- Icy Hot Menthol Medicine Pain Relief Patch
- Heating Pain Relief Patches for Menstrual Cramps
- Far Infrared Heat Pain Relief Patches Transdermal Patches
People Also Ask
- How do pain relief patches provide targeted relief? Discover the Science Behind Effective Pain Management
- How do pain relief patches compare to other pain relief methods? Discover Targeted, Long-Lasting Relief
- What are pain relief patches and how are they used? A Guide to Safe, Targeted Relief
- How often should pain relief patches be used? Get the Right Schedule for Targeted Relief
- How quickly does the Deep Heat Pain Relief Back Patch activate and how long does it provide warmth? Get 16-Hour Relief














