A buprenorphine patch is a transdermal opioid medication designed to treat severe, long-term pain that requires continuous, around-the-clock management. It works by delivering the drug buprenorphine slowly through the skin into the bloodstream. Once in the body, it binds to opioid receptors in the central nervous system, effectively blocking pain signals from reaching the brain and altering the body's perception of pain.
The core purpose of a buprenorphine patch is to provide a steady, consistent level of pain relief over several days. It is specifically intended for managing persistent, chronic pain and is fundamentally unsuitable for treating sudden or acute pain.

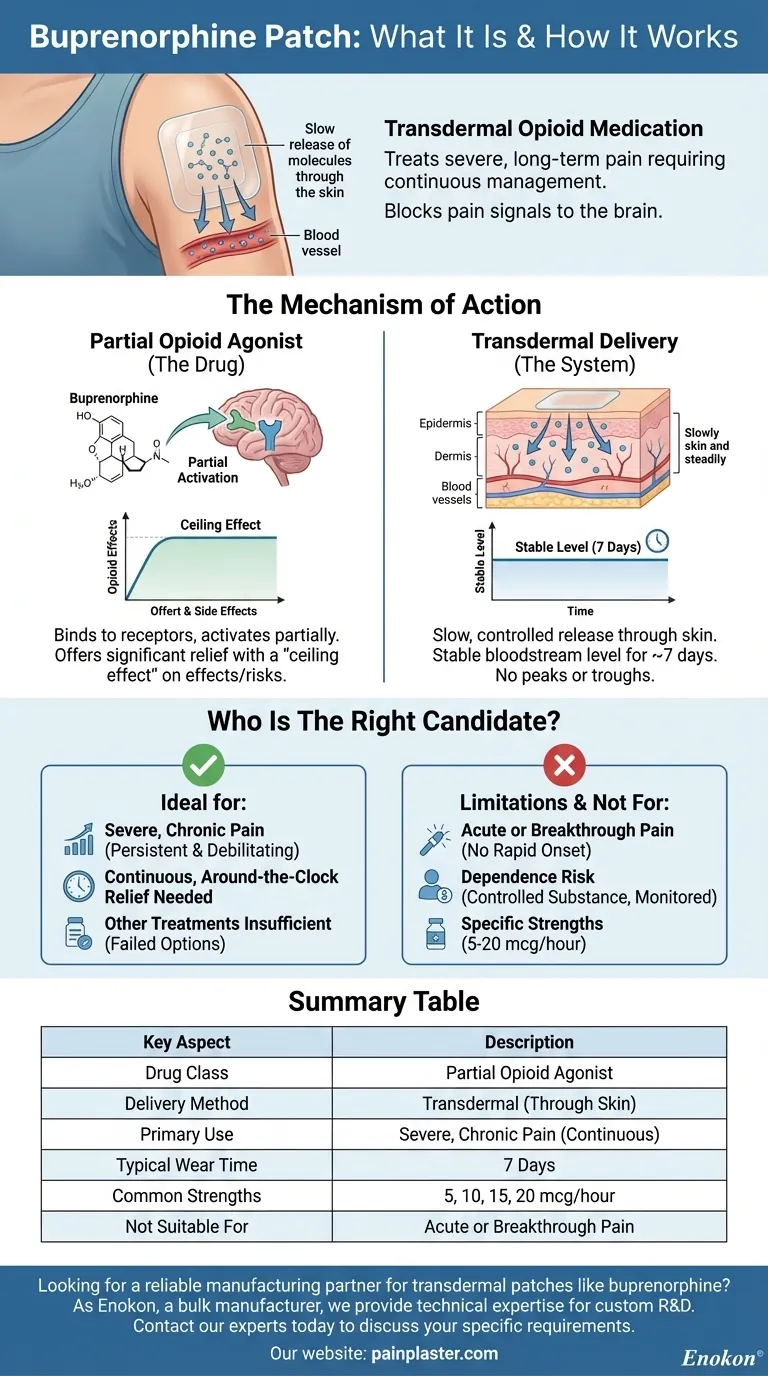
The Mechanism of Action: A Deeper Look
Understanding how the buprenorphine patch functions requires looking at both the drug itself and its delivery method. These two factors define its specific role in pain management.
A Partial Opioid Agonist
Buprenorphine belongs to a class of medicines called partial opioid agonists. Unlike full agonists (like morphine or oxycodone) which fully activate opioid receptors, buprenorphine binds to these receptors but only activates them partially.
This partial activation is a key characteristic. It provides significant pain relief while often having a "ceiling effect," meaning its opioid effects tend to plateau even with increased doses. This can potentially lower the risk of certain side effects compared to full agonists.
The Transdermal Delivery System
The patch is a transdermal system, which means the medication is absorbed directly through the skin. This method is designed for a slow and controlled release.
After applying a patch, it can take many hours for the medication to reach a stable level in the bloodstream. The patch is typically worn for seven days, providing a continuous infusion of buprenorphine throughout that entire period. This eliminates the peaks and troughs associated with taking oral, short-acting pain medication.
Who is the Right Candidate for This Treatment?
The buprenorphine patch is not a first-line treatment. Its use is reserved for very specific clinical situations where other options have proven inadequate.
Indication: Severe and Chronic Pain
The primary indication is for pain that is both severe in intensity and chronic in nature. This is not for intermittent headaches or the pain from a minor injury. It is for conditions that cause persistent, debilitating pain.
When Other Treatments are Insufficient
A healthcare provider typically considers this patch only after other pain management strategies have failed. This includes non-opioid medications, other types of analgesics, or when other opioids cannot be tolerated due to side effects.
The Need for Around-the-Clock Relief
The ideal candidate requires stable, continuous pain control. The patch's long-acting nature is its main advantage, making it suitable for patients whose pain is constant and disruptive throughout the day and night.
Understanding the Trade-offs and Limitations
While effective for its specific purpose, the buprenorphine patch comes with critical limitations that must be understood.
Not for Acute or "As-Needed" Pain
Because of its slow onset, the patch is completely ineffective for acute pain (like post-surgical pain or a broken bone) or for "breakthrough" pain that flares up suddenly. It cannot provide rapid relief.
Potential for Dependence
As an opioid, buprenorphine carries a risk of physical dependence. It is a controlled substance, and its use must be carefully monitored by a healthcare professional to manage this risk.
Specific Dosage Strengths
In the United States, buprenorphine patches are available in several strengths, typically ranging from 5 to 20 mcg/hour. The correct dose is determined by a physician based on the patient's pain level and history with other opioid medications.
Making the Right Choice for Your Goal
Discussing any pain treatment with your healthcare provider is crucial. Understanding the intended use of this specific medication helps you have a more informed conversation.
- If your primary focus is managing stable, chronic pain: The patch's slow, continuous delivery may provide consistent relief without the peaks and valleys of short-acting medications.
- If you need relief for sudden, intermittent, or 'breakthrough' pain: This patch is not suitable, and alternative or supplementary medications are required for immediate effect.
- If your goal is to find an alternative after other opioids were not tolerated: Buprenorphine's unique properties as a partial agonist might offer a different balance of pain relief and side effects.
Ultimately, knowing how this specialized tool works empowers you to partner with your doctor to build the most effective pain management strategy for your specific condition.
Summary Table:
| Key Aspect | Description |
|---|---|
| Drug Class | Partial Opioid Agonist |
| Delivery Method | Transdermal (Through the Skin) |
| Primary Use | Severe, Chronic Pain (Around-the-Clock) |
| Typical Wear Time | 7 Days |
| Common Strengths | 5, 10, 15, 20 mcg/hour |
| Not Suitable For | Acute or Breakthrough Pain |
Looking for a reliable manufacturing partner for transdermal patches like buprenorphine?
As Enokon, a bulk manufacturer of reliable transdermal patches and pain plasters, we provide healthcare and pharma distributors and brands with the technical expertise for custom R&D and development. Benefit from our experience to bring your pain management solutions to market efficiently.
Contact our experts today to discuss your specific requirements.
Visual Guide
Related Products
- Far Infrared Deep Heat Relief Patches Medicated Pain Relief Patches
- Far Infrared Heat Pain Relief Patches Transdermal Patches
- Mugwort Wormwood Pain Relief Patch for Neck Pain
- Icy Hot Menthol Medicine Pain Relief Patch
- Menthol Gel Pain Relief Patch
People Also Ask
- How quickly does the Deep Heat Pain Relief Back Patch activate and how long does it provide warmth? Get 16-Hour Relief
- How do pain relief patches provide targeted relief? Discover the Science Behind Effective Pain Management
- How do pain relief patches compare to other pain relief methods? Discover Targeted, Long-Lasting Relief
- How do pain relief patches work? A Guide to Targeted, Long-Lasting Pain Relief
- How do Deep Heat Pain Relief Patches provide pain relief? Discover the Drug-Free Mechanism















