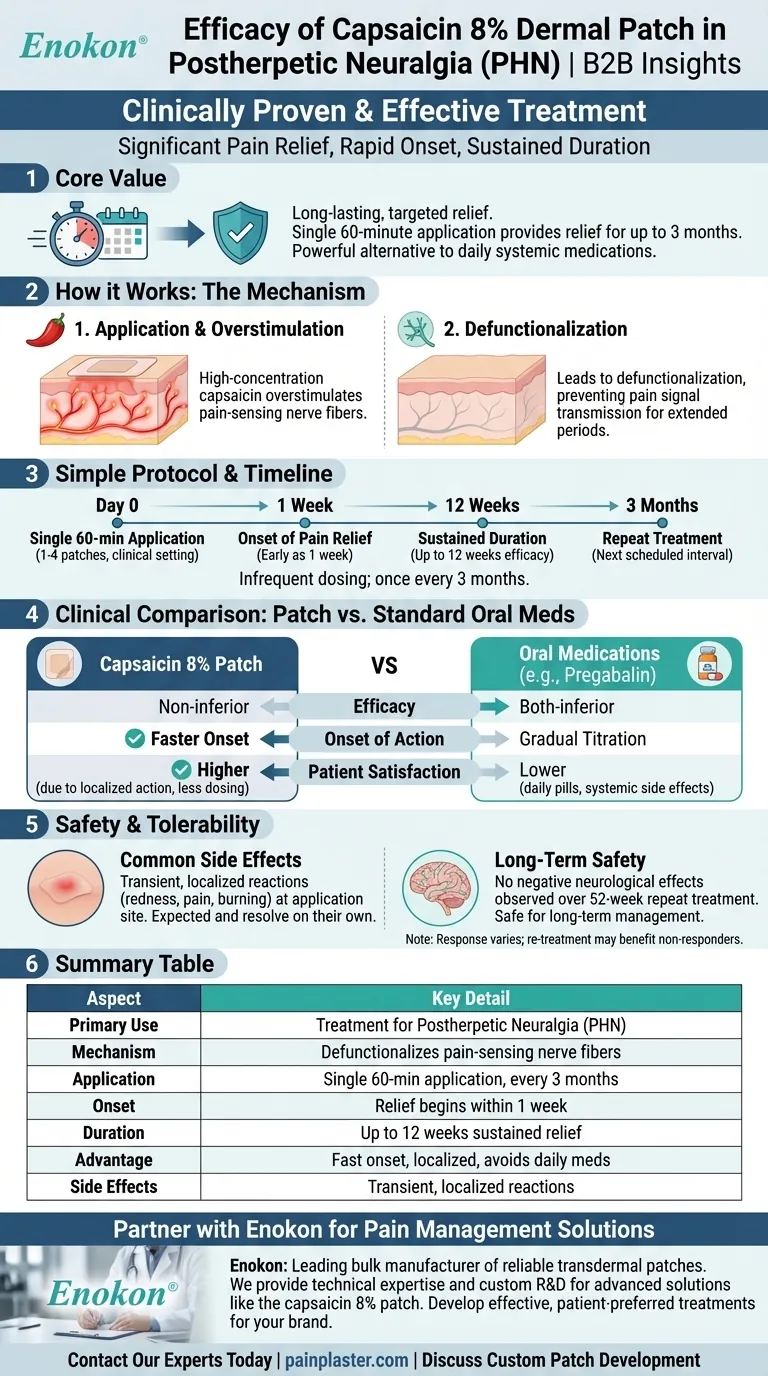
The capsaicin 8% dermal patch is a clinically proven and effective treatment for providing significant pain relief in patients with postherpetic neuralgia (PHN). A single, 60-minute application can deliver rapid and sustained pain reduction that lasts for up to three months. Its efficacy is comparable to standard oral medications, but it often works faster and with higher patient satisfaction due to its localized action and infrequent dosing schedule.
The core value of the capsaicin 8% patch lies in its ability to provide long-lasting, targeted relief from nerve pain with a single application every three months, offering a powerful alternative to the burden of daily systemic medications.

How the Capsaicin 8% Patch Delivers Relief
The Unique Mechanism of Action
The patch contains a high concentration of capsaicin, the compound found in chili peppers. When applied to the skin, it selectively targets and overstimulates pain-sensing nerve fibers. This initial stimulation can cause a temporary burning sensation but ultimately leads to a "defunctionalization" of these fibers, making them unable to transmit pain signals for an extended period.
A Simple and Infrequent Protocol
Treatment for postherpetic neuralgia involves a single, 60-minute application of up to four patches directly over the most painful areas of intact skin. This procedure is typically performed in a clinical setting and is only required once every three months.
Onset and Duration of Efficacy
Patients may begin to experience pain relief as early as one week after the first treatment. Studies confirm that a single application provides sustained pain reduction for up to 12 weeks. Furthermore, repeat treatments over a 52-week period have demonstrated continued efficacy without loss of effect.
A Clinical Comparison to Standard Treatments
Efficacy vs. Oral Medications
In clinical trials, the capsaicin 8% patch was found to be non-inferior to oral pregabalin, a commonly prescribed medication for neuropathic pain. This means it provides a similar level of pain relief.
A Faster Onset of Action
A key advantage of the patch is its faster onset of action. Patients often feel relief more quickly than with oral medications that need to be gradually titrated up to an effective dose.
Higher Patient Satisfaction
The localized nature of the treatment and the infrequent dosing schedule contribute to greater treatment satisfaction compared to daily oral therapies. This avoids the need to remember daily pills and minimizes systemic side effects.
Understanding the Trade-offs and Side Effects
Common Application-Site Reactions
The capsaicin 8% patch is generally well-tolerated. The most common adverse events are transient, localized reactions at the application site, such as temporary redness, pain, or a burning sensation. These effects are expected and typically resolve on their own.
Long-Term Neurological Safety
A primary concern with any nerve-targeting treatment is long-term safety. Studies involving repeat treatments over a full year found no negative neurological effects compared to standard care alone, confirming its safety profile for long-term management.
Not a Universal Response
It is important to note that not all patients respond to the first treatment. However, some who do not find relief initially may benefit from a second application at the next scheduled interval.
Making the Right Choice for Your Goal
- If your primary focus is rapid relief and avoiding daily medication: The capsaicin 8% patch is an excellent option, as its fast onset and quarterly application bypass the need for daily oral drugs.
- If your primary focus is minimizing systemic side effects: This patch is a strong alternative, as its effects are localized, avoiding the widespread side effects common with oral neuropathic pain medications.
- If your primary focus is a sustainable, long-term strategy: The evidence supports repeated use over a year, showing sustained pain relief without adverse neurological impact, making it a viable long-term treatment.
By delivering highly concentrated medication directly to the source of the pain, the capsaicin 8% patch offers a powerful and well-tolerated approach to managing postherpetic neuralgia.
Summary Table:
| Aspect | Key Detail |
|---|---|
| Primary Use | Treatment for Postherpetic Neuralgia (PHN) |
| Mechanism | Defunctionalizes pain-sensing nerve fibers |
| Application | Single 60-minute application, once every 3 months |
| Onset of Action | Relief can begin within 1 week |
| Duration of Effect | Sustained pain reduction for up to 12 weeks |
| Key Advantage | Fast onset, localized action, avoids daily systemic medication |
| Common Side Effects | Transient, localized reactions (redness, pain) |
Ready to offer your patients a powerful, long-lasting solution for neuropathic pain?
As Enokon, a leading bulk manufacturer of reliable transdermal patches, we provide the technical expertise and custom R&D capabilities to help healthcare and pharma brands develop advanced pain management solutions like the capsaicin 8% patch. Benefit from our experience to create effective, patient-preferred treatments.
Contact our experts today to discuss your custom patch development needs.
Visual Guide
Related Products
- Capsaicin Chili Medicated Pain Relief Patches
- Heat Relief Capsicum Patch for Lower Back Pain Relief
- Far Infrared Deep Heat Relief Patches Medicated Pain Relief Patches
- Heating Pain Relief Patches for Menstrual Cramps
- Menthol Gel Pain Relief Patch
People Also Ask
- Can pregnant women use pain relief patches? Your Essential Guide to Safe Pain Management
- How do pain relief patches work? A Guide to Targeted, Long-Lasting Pain Relief
- What precautions should be taken with buprenorphine patches? Ensure Safe Use and Avoid Overdose Risks
- Can children use the pain relief patch? A Critical Safety Guide for Parents
- How do you apply the Signal Relief patch to find the proper placement? A Step-by-Step Guide to Maximum Relief
















