The pressure-sensitive adhesive (PSA) layer in a transdermal drug delivery system must successfully execute a dual role: mechanical fixation and pharmacokinetic regulation. Mechanically, it requires sufficient initial tack and cohesive strength to maintain continuous, secure contact with the skin throughout the administration period without causing irritation. Functionally, it often acts as the drug reservoir, where specific chemical properties—such as polarity and cross-linking density—directly control the migration and release rate of the active ingredients.
Core Insight: The adhesive is not merely a passive fastener; it is an active component of the drug delivery matrix. A successful PSA formulation must balance the physical requirement of keeping the patch in place with the chemical requirement of releasing the drug at a controlled rate, all while maintaining strict biocompatibility.
Mechanical Performance: The Foundation of Efficacy
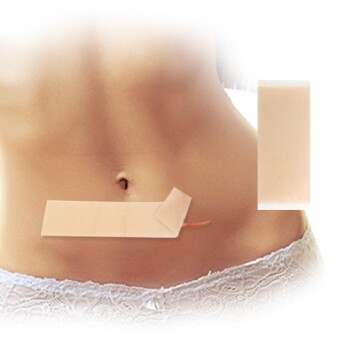
The primary function of the PSA is to establish a secure interface between the device and the biological barrier (the stratum corneum). Without this, drug delivery is impossible.
Initial Tack and Cohesive Strength
The adhesive must bond firmly to the skin under light pressure immediately upon application.
It requires high cohesive strength to ensure the patch remains attached during movement or friction. If the adhesive layer fails mechanically, the diffusion pathway is broken, and the therapeutic effect ceases.
Continuous Contact for Diffusion
The patch must maintain tight, uninterrupted contact with the skin surface.
Gaps or lifting in the adhesive layer prevent the drug molecules from partitioning effectively into the skin. This contact is the absolute prerequisite for a successful diffusion pathway.
Clean Removability
While adhesion must be strong, the PSA must be removable without leaving residue.
It must also detach without causing mechanical trauma to the skin, striking a balance between secure fixation and gentle removal.
Biological Compatibility and Safety
Because transdermal patches are often worn for extended periods (up to 24 hours or more), the interaction between the adhesive and the skin is critical.
Low Allergenicity and Biocompatibility
The adhesive formulation must be chemically inert regarding the skin environment.
It must demonstrate excellent biocompatibility to minimize the risk of allergic reactions or contact dermatitis during long-term wear.
Chemical Stability
The adhesive must remain chemically stable when in contact with active pharmaceutical ingredients (APIs) and permeation enhancers.
It must resist aging or degradation during the product's shelf life, ensuring that the adhesive properties do not deteriorate over time.
Drug Release Kinetics
In many system designs, the adhesive serves as the drug reservoir or diffusion matrix. Its physicochemical properties dictate how the drug moves from the patch into the body.
Regulating Migration via Cross-Linking
The cross-linking density of the adhesive matrix is a critical variable.
A tighter network (higher density) can restrict the movement of large molecules, effectively slowing the migration rate of the active ingredients to the skin surface.
Polarity and Solubility
The polarity of the adhesive directly influences the drug's solubility and diffusion coefficient.
The chemical environment of the adhesive determines how easily the drug dissolves within the matrix and how readily it partitions out of the adhesive and into the skin.
Understanding the Trade-offs
Designing a PSA layer involves inherent contradictions that must be managed.
Adhesion vs. Drug Release
Increasing the cohesive strength (often via cross-linking) improves mechanical stability but can hinder drug mobility.
An overly dense matrix may "trap" the drug, reducing the bioavailability and altering the intended release profile.
Tack vs. Skin Irritation
Formulations with extremely high initial tack provide the best security against falling off but increase the risk of skin damage upon removal.
Furthermore, aggressive adhesives may occlude the skin too heavily, leading to irritation from moisture accumulation or chemical interaction over long dosing cycles.
Making the Right Choice for Your Goal
The "ideal" adhesive depends on the specific therapeutic requirements of your drug and the intended wear duration.
- If your primary focus is Controlled Release: Prioritize the polarity and cross-linking density of the adhesive to finetune the diffusion coefficient and ensure a constant delivery rate.
- If your primary focus is Long-Term Wear (e.g., 24+ hours): Prioritize biocompatibility and cohesive strength to prevent irritation and ensure the patch does not lift during sleep or activity.
- If your primary focus is Shelf-Life Stability: Prioritize physicochemical compatibility to ensure the adhesive does not react with the drug or permeation enhancers over time.
Ultimately, the optimal pressure-sensitive adhesive must be engineered to hold the device firmly in place while simultaneously letting the drug molecules go.
Summary Table:
| Performance Category | Key Criteria | Core Function |
|---|---|---|
| Mechanical | Tack, Cohesion, Removability | Ensures continuous skin contact and residue-free removal. |
| Biological | Biocompatibility, Low Irritation | Minimizes allergic reactions and skin trauma during long-term wear. |
| Pharmacokinetic | Cross-linking, Polarity | Controls drug solubility and regulates the release rate/migration. |
| Stability | Chemical Compatibility | Prevents degradation when mixed with APIs or permeation enhancers. |
Partner with Enokon for Expert Transdermal Solutions
Are you looking to optimize the adhesive performance of your next product? As a trusted manufacturer and wholesale partner, Enokon specializes in high-quality transdermal drug delivery systems—excluding microneedle technology.
We offer a comprehensive range of solutions, including Lidocaine, Menthol, Capsicum, Herbal, and Far Infrared pain relief patches, alongside specialized products like Eye Protection, Detox, and Medical Cooling Gel patches. Whether you need custom R&D or wholesale manufacturing, our team ensures your patches meet the highest standards of adhesion and drug release kinetics.
Ready to elevate your product line? Contact us today to discuss your custom R&D needs!
References
- V. K. Singla. Exploring Transdermal Delivery of Traditional Herbal Medicine for Central Nervous System Disorders. DOI: 10.56025/ijaresm.2023.1201241700
This article is also based on technical information from Enokon Knowledge Base .
Related Products
- Menthol Gel Pain Relief Patch
- Lidocaine Hydrogel Pain Relief Patch for Pain Relief
- Icy Hot Menthol Medicine Pain Relief Patch
- Mugwort Wormwood Pain Relief Patch for Neck Pain
- Asthma Cough and Pain Relief Patch for Adults and Kids
People Also Ask
- What are the serious side effects of menthol patch that require immediate medical attention?
- What important precautions should be taken with menthol topical? Safety Guide for Effective Use
- How does menthol function as a topical analgesic? The Science Behind Cooling Pain Relief
- What should be done if a dose of menthol patch is missed? Key Steps for Safe Use
- What should be avoided while using a menthol patch? Key Safety Tips for Effective Pain Relief