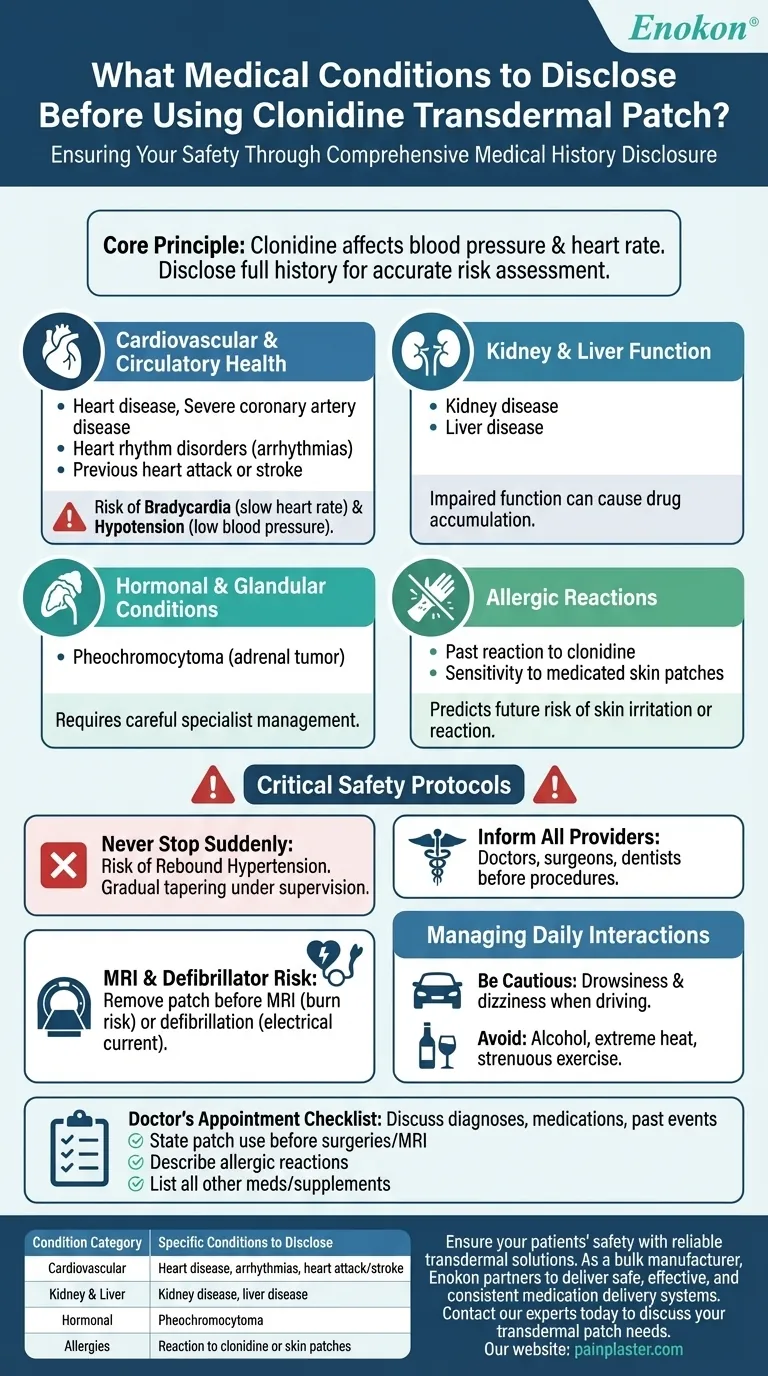
Before using a clonidine transdermal patch, you must inform your doctor about a comprehensive set of medical conditions, primarily those related to your cardiovascular and renal systems. This includes any history of heart disease, severe coronary artery disease, heart rhythm disorders, previous heart attack or stroke, kidney disease, and a specific adrenal gland tumor called pheochromocytoma. It is also critical to disclose any past allergic reactions to clonidine or other medicated skin patches.
The core principle is this: Clonidine is a powerful medication that systemically affects your blood pressure and heart rate. Disclosing your full medical history allows your doctor to accurately weigh the therapeutic benefits against the potential risks for your specific health profile.
Why Your Medical History is Critical
Clonidine works by acting on the central nervous system to relax blood vessels and slow the heart rate, thereby lowering blood pressure. Because its effects are widespread, pre-existing conditions in certain organ systems can significantly alter how your body responds to the medication, increasing the risk of adverse events.
Full disclosure is not just a formality; it is the primary tool your doctor uses to ensure your safety and the effectiveness of the treatment.
Key Conditions to Discuss with Your Doctor
Organize your medical history to ensure you cover these critical areas during your consultation.
Cardiovascular and Circulatory Health
This is the most important category. Clonidine directly manipulates the cardiovascular system.
Inform your doctor about any history of:
- Heart disease or severe coronary artery disease
- Heart rhythm disorders (arrhythmias)
- Previous heart attack or stroke
Because clonidine slows the heart rate and lowers blood pressure, these conditions can increase your risk of complications like an abnormally slow heart rate (bradycardia) or dangerously low blood pressure (hypotension).
Kidney and Liver Function
Your body must be able to process and eliminate the medication effectively.
Disclose any diagnosis of kidney disease or liver disease. These organs are responsible for filtering and clearing clonidine from your bloodstream. Impaired function can cause the drug to accumulate to potentially toxic levels.
Hormonal and Glandular Conditions
Certain tumors can have unpredictable interactions with blood pressure medications.
Specifically mention if you have ever been diagnosed with pheochromocytoma. This is a tumor of the adrenal gland that can cause severe high blood pressure, and clonidine's effects in this context require careful specialist management.
History of Allergic Reactions
Your body's past responses are a key predictor of future ones.
Report any allergic reaction you have ever had to clonidine in any form. You should also mention any known sensitivity or allergic reactions to other medicated skin patches, as this can indicate a higher likelihood of skin irritation or a more severe reaction.
Beyond Pre-existing Conditions: Critical Safety Protocols
Safe use of clonidine extends beyond your initial diagnosis. You must be aware of several operational safety rules.
The Danger of Abruptly Stopping
Never stop using the clonidine patch suddenly. Doing so can cause a rapid, dangerous increase in blood pressure known as "rebound hypertension." Your doctor must supervise a gradual tapering process to discontinue the medication safely.
Informing All Healthcare Providers
Any professional treating you must know you use this patch. This includes doctors, surgeons, and dentists before any procedure.
The MRI and Defibrillator Risk
The clonidine patch contains a small amount of aluminum. You must remove the patch before an MRI scan to prevent the risk of skin burns at the patch site.
Similarly, if emergency heart resuscitation is needed, the patch must be removed before using a defibrillator to ensure the electrical current is delivered effectively and safely.
Managing Daily Interactions
Be aware that clonidine can cause drowsiness and dizziness. Be cautious when driving or operating machinery. Using alcohol, exposure to extreme heat, or strenuous exercise can amplify these effects and further lower your blood pressure.
A Checklist for Your Doctor's Appointment
Use this guide to ensure you have a productive and safe consultation with your physician.
- If you have any history of heart, blood pressure, or kidney issues: Be prepared to discuss your specific diagnoses, all medications you take for them, and any past events like a heart attack.
- If you are scheduled for any surgery or medical procedure (including an MRI): State clearly that you use a clonidine patch and ask for precise instructions on when to remove and reapply it.
- If you have ever had an allergic reaction to any medication or skin patch: Describe the reaction in detail so your doctor can assess the risk of a similar reaction.
- If you are taking any other medications, supplements, or over-the-counter drugs: Provide a complete list to screen for potential drug interactions that could alter clonidine's effectiveness or safety.
Open and thorough communication with your healthcare provider is the single most important factor in ensuring your treatment is both safe and successful.
Summary Table:
| Condition Category | Specific Conditions to Disclose |
|---|---|
| Cardiovascular | Heart disease, severe coronary artery disease, heart rhythm disorders, previous heart attack or stroke |
| Kidney & Liver | Kidney disease, liver disease |
| Hormonal | Pheochromocytoma (adrenal gland tumor) |
| Allergies | Any allergic reaction to clonidine or other medicated skin patches |
Ensure your patients' safety with reliable transdermal solutions.
As a bulk manufacturer of high-quality transdermal patches, Enokon partners with healthcare and pharmaceutical distributors and brands to deliver safe, effective, and consistent medication delivery systems. Our technical expertise supports custom R&D and development to meet your specific requirements, ensuring the highest standards of quality and patient safety.
Contact our experts today to discuss your transdermal patch needs and benefit from our reliable manufacturing and development capabilities.
Visual Guide
Related Products
- Far Infrared Heat Pain Relief Patches Transdermal Patches
- Far Infrared Deep Heat Relief Patches Medicated Pain Relief Patches
- Heating Pain Relief Patches for Menstrual Cramps
- Herbal Eye Protection Patch Eye Patch
- Asthma Cough and Pain Relief Patch for Adults and Kids
People Also Ask
- What are the common side effects of using the medicated heat patch? Understanding Risks & Safe Use
- How does the Deep Heat Back Patch work? A Drug-Free Solution for Targeted Pain Relief
- What did the UK Million Women Study find regarding transdermal versus oral hormone therapy? A Safer Choice for Gallbladder Health
- Can heat patches be used for fresh injuries? Avoid This Common Mistake for Faster Recovery
- What are the key features of the Deep Heat Pain Relief Back Patch? Get Up to 16 Hours of Drug-Free Relief














