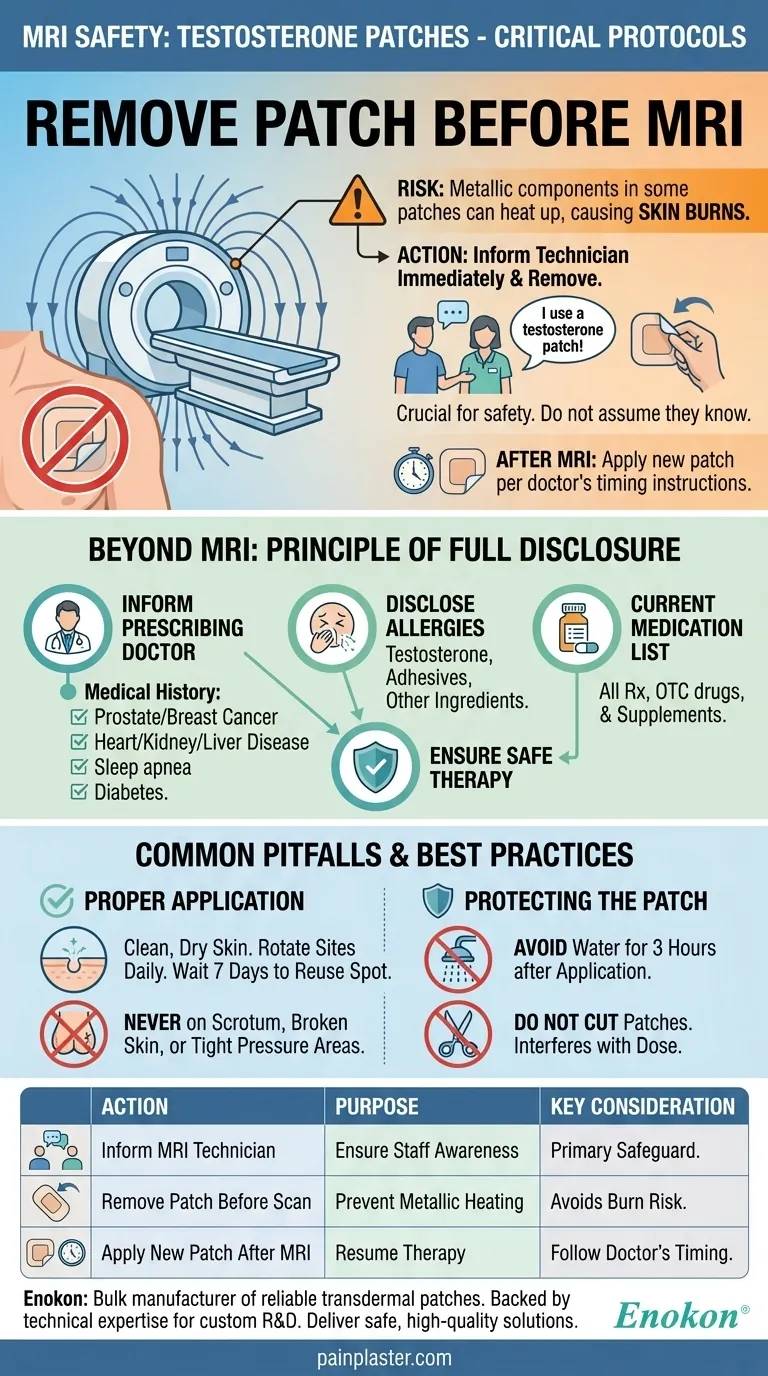
Before undergoing an MRI, you must remove your testosterone patch. This is a critical safety step because some patches contain metallic components that can heat up during the scan, potentially causing skin burns at the application site. Always inform the MRI technician or a member of your care team that you use a testosterone patch so they can confirm it has been removed.
The immediate action is to remove the patch to prevent injury during the MRI. However, this specific instruction is part of a larger, more fundamental principle: ensuring your safety requires transparent and continuous communication about your treatment with all of your healthcare providers.

The Critical Pre-MRI Safety Protocol
The interaction between an MRI's powerful magnetic fields and certain medical devices is a significant safety concern. Transdermal patches fall into this category.
Inform Your MRI Technician Immediately
Your first and most important step is to tell the staff conducting the procedure that you are using a testosterone patch. Do not assume they will know or that it is irrelevant.
This simple act of communication is the primary safeguard against potential complications.
Why Removal is Non-Negotiable
Many transdermal patches, including some brands of testosterone, contain trace amounts of metal in their foil backing or adhesive layers.
When exposed to the MRI's magnetic fields, these metallic components can heat up rapidly. This poses a direct risk of a second or third-degree burn on the skin beneath the patch.
After the MRI is Complete
Once your procedure is finished, you can apply a new patch. Follow the timing instructions provided by your doctor or pharmacist for reapplication to maintain your prescribed dose schedule.
Beyond the MRI: The Principle of Full Disclosure
The need to inform an MRI technician is a single instance of a broader rule for safe testosterone therapy. Your entire medical team must have a complete picture of your health.
Informing Your Prescribing Doctor
Before you even begin therapy, your doctor must be aware of your complete medical history.
Be certain to disclose conditions such as prostate or breast cancer, heart, kidney, or liver disease, sleep apnea, diabetes, or issues with urination. This information is vital for determining if the therapy is safe for you.
Disclosing All Allergies
It is critical to report any known allergies. This includes not just an allergy to testosterone itself, but also to the adhesives used in the patch or any other ingredients.
Keeping a Current Medication List
Provide your doctor with a comprehensive list of all medications you take, including over-the-counter drugs and supplements. This helps prevent dangerous drug interactions.
Common Pitfalls and Best Practices
Proper use of the patch is just as important as medical disclosure for ensuring your safety and the treatment's effectiveness.
Proper Application Technique
Always apply the patch to a clean, dry area of skin. Rotate application sites each day and wait at least seven days before reusing a spot to prevent skin irritation.
Never apply patches to the scrotum, to broken or irritated skin, or to areas that will be under tight pressure from clothing.
Protecting the Patch
For at least three hours after applying a new patch, you should avoid showering, swimming, or bathing. This allows the adhesive to set properly and ensures the medication is absorbed.
Do not cut the patches, as this can interfere with the dose delivery mechanism.
Making the Right Choice for Your Goal
Navigating medical treatments requires you to be an active and informed participant in your own care.
- If your primary focus is preparing for an MRI or surgery: Your immediate action is to inform the technician and remove the patch before the procedure begins.
- If your primary focus is managing ongoing therapy safely: Your priority is to maintain a completely transparent dialogue with your doctor about your health history, allergies, and any new symptoms.
- If your primary focus is getting the most out of your daily treatment: Your goal is to adhere strictly to the prescribed application and management protocols to ensure consistent dosing and avoid skin issues.
Proactive communication is the cornerstone of safe and effective medical treatment.
Summary Table:
| Action | Purpose | Key Consideration |
|---|---|---|
| Inform MRI Technician | Ensure staff is aware of the patch. | Primary safeguard against complications. |
| Remove Patch Before Scan | Prevent metallic components from heating up. | Avoids risk of second or third-degree burns. |
| Apply New Patch After MRI | Resume prescribed therapy. | Follow doctor/pharmacist timing for dose consistency. |
Ensure your transdermal patches are safe and effective. As a bulk manufacturer of reliable transdermal patches and pain plasters, Enokon provides healthcare and pharma distributors and brands with products backed by technical expertise for custom R&D and development. Let us help you deliver safe, high-quality solutions to your customers.
Contact our experts today to discuss your needs.
Visual Guide
Related Products
- Prostate Pain Kidney Health Care Patch for Men
- Capsaicin Chili Medicated Pain Relief Patches
- Far Infrared Deep Heat Relief Patches Medicated Pain Relief Patches
- Heating Pain Relief Patches for Menstrual Cramps
- Herbal Eye Protection Patch Eye Patch
People Also Ask
- What precautions should be taken when applying testosterone patches? Maximize Safety and Effectiveness
- What should be done if a testosterone patch is missed or falls off? Follow these simple timing rules for safety and consistency.
- What is the purpose of testosterone patches? A Steady Solution for Low Testosterone
- What should be done in case of a testosterone patch overdose? A Step-by-Step Emergency Guide
- How often should testosterone patches be applied? Daily Dosage & Best Practices













