If your buprenorphine patch comes off or is causing skin irritation, the correct immediate action is to remove the patch and apply a new one to a different, clean area of your skin. This ensures you maintain a consistent dose of your medication, which is critical for its effectiveness.
The core principle of managing a transdermal patch is to ensure uninterrupted, correct dosing while protecting your skin's health. Always prioritize replacing a compromised patch over trying to make a faulty one work, and never ignore signs of significant skin irritation.

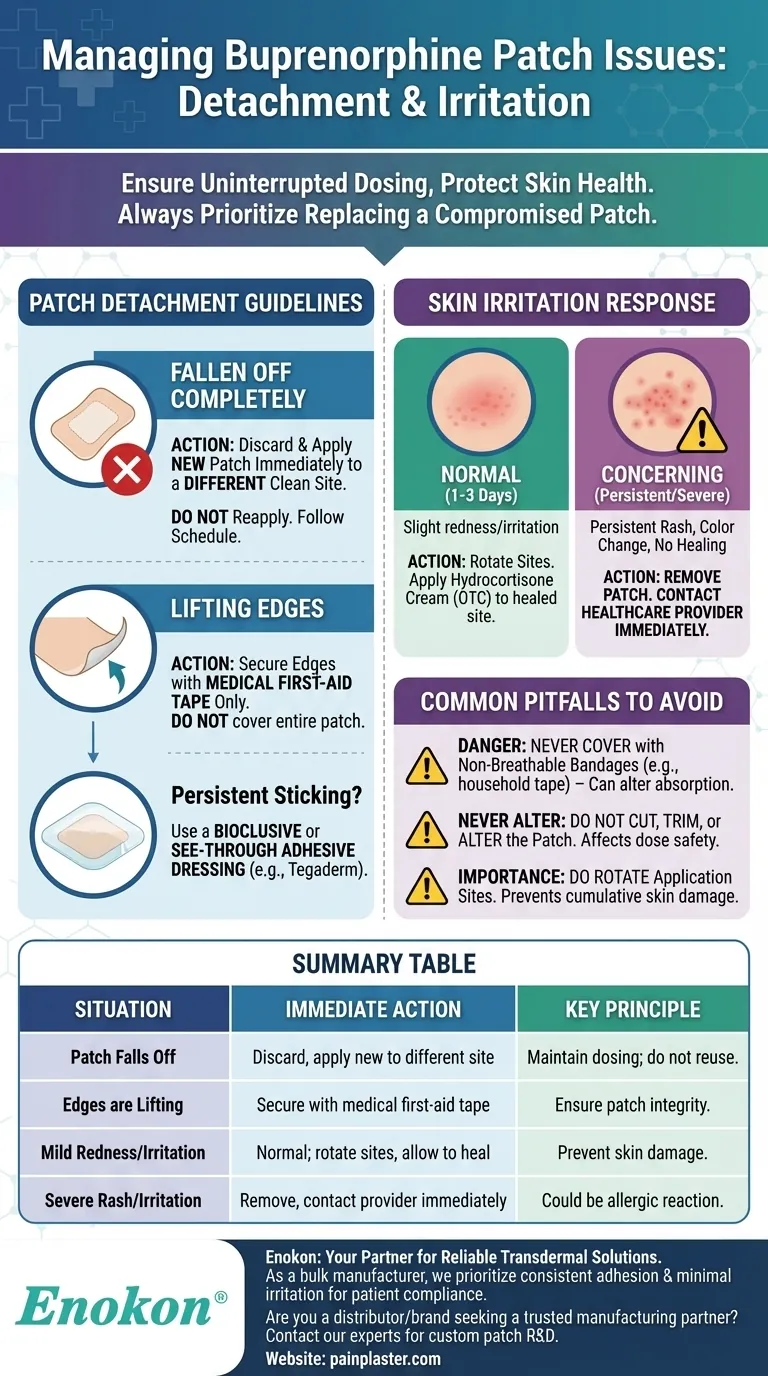
Managing a Detached or Loose Patch
Maintaining the patch's adhesion is essential for the medication to be absorbed correctly. If you encounter issues, a specific protocol must be followed.
The Immediate Action: Replace and Relocate
If a patch comes off entirely, do not attempt to reapply it. The adhesive will be compromised, and you cannot be sure of its integrity.
Immediately apply a brand-new patch to a different, clean, dry, and hairless skin site. Continue to follow your original schedule for changing the patch.
Securing Lifting Edges
If only the edges of the patch begin to lift, you can secure them. Use a standard first-aid tape applied only over the edges to press them firmly back against the skin.
For Persistent Sticking Problems
If you consistently have trouble with adhesion, you may cover the entire patch with a specific type of dressing. Use a bioclusive or see-through adhesive dressing (like Tegaderm). These are designed to be breathable and will not interfere with medication delivery.
Responding to Skin Irritation
It's important to distinguish between a normal, temporary skin reaction and a more serious issue that requires medical attention.
Differentiating Normal vs. Concerning Irritation
It is normal for the skin to be slightly red or feel irritated for one to three days after you remove a patch. This is a common reaction to the adhesive and the medication.
However, if you develop a persistent rash, experience skin color changes, or the irritation does not begin to heal after a few days, this is not normal and should be addressed.
How to Manage Mild Irritation
For mild, expected redness, simply ensure your next patch is applied to a different location. After removing a patch from an irritated site, you can apply a small amount of over-the-counter hydrocortisone cream to help it heal.
When to Contact Your Healthcare Provider
Contact your provider immediately if you develop a severe rash or notice significant skin color changes at the application site. This could indicate an allergic reaction, and you may need to stop using the patch.
Common Pitfalls to Avoid
Improperly managing your patch can lead to incorrect dosing or skin damage. Avoiding these common mistakes is critical for your safety and the treatment's success.
The Danger of Improper Coverings
Never cover the patch with standard bandages, household tape, or any non-breathable dressing. These materials can trap heat, which may alter the rate at which the medication is absorbed into your body, leading to a potentially dangerous dosage. Stick only to the recommended first-aid tape for edges or specialized see-through dressings.
Never Alter or Trim the Patch
Do not cut, trim, or alter a buprenorphine patch in any way. The patch is designed as a complete system to deliver a specific dose over time. Cutting it can damage this system and lead to unpredictable and unsafe medication release.
The Importance of Site Rotation
To prevent cumulative skin irritation, you must rotate application sites. Applying a new patch to the same spot repeatedly will almost certainly lead to skin breakdown and discomfort. Always choose a fresh site for each new patch.
Making the Right Choice for Your Situation
Your response should be guided by the specific problem you are facing.
- If your patch falls off completely: Discard it safely and apply a new patch to a different site immediately.
- If the edges of your patch are lifting: Secure them with a small amount of medical first-aid tape.
- If you have mild redness after removing a patch: This is expected; allow the area to heal and apply the next patch elsewhere.
- If you develop a rash or severe, persistent irritation: Remove the patch, do not apply a new one, and contact your doctor for guidance.
Following these guidelines ensures your buprenorphine treatment remains as safe and effective as possible.
Summary Table:
| Situation | Immediate Action | Key Principle |
|---|---|---|
| Patch Falls Off | Discard and apply a new patch to a different, clean skin site. | Maintain consistent dosing; do not reuse. |
| Edges are Lifting | Secure edges only with medical first-aid tape. | Ensure patch integrity for correct absorption. |
| Mild Redness/Irritation | This is often normal. Rotate application sites and allow skin to heal. | Prevent cumulative skin damage. |
| Severe Rash/Persistent Irritation | Remove the patch and contact your healthcare provider immediately. | Could indicate an allergic reaction requiring medical attention. |
Ensure the reliability and comfort of your transdermal therapy.
As Enokon, a bulk manufacturer of reliable transdermal patches and pain plasters, we understand that consistent, high-quality adhesion and minimal skin irritation are paramount for patient compliance and treatment success. Our technical expertise in custom R&D and development ensures that every patch delivers precise, safe, and effective medication.
Are you a healthcare or pharmaceutical distributor or brand looking for a trusted manufacturing partner? Let us help you develop superior transdermal solutions that enhance patient outcomes.
Contact our experts today to discuss your custom patch requirements.
Visual Guide
Related Products
- Far Infrared Deep Heat Relief Patches Medicated Pain Relief Patches
- Far Infrared Heat Pain Relief Patches Transdermal Patches
- Mugwort Wormwood Pain Relief Patch for Neck Pain
- Icy Hot Menthol Medicine Pain Relief Patch
- Menthol Gel Pain Relief Patch
People Also Ask
- How should pain relief patches be applied and used? A Guide to Safe & Effective Targeted Relief
- How does the Deep Heat Back Patch work? A Drug-Free Solution for Targeted Pain Relief
- How do pain relief patches compare to other pain relief methods? Discover Targeted, Long-Lasting Relief
- How quickly does the Deep Heat Pain Relief Back Patch activate and how long does it provide warmth? Get 16-Hour Relief
- What are pain relief patches and how are they used? A Guide to Safe, Targeted Relief














