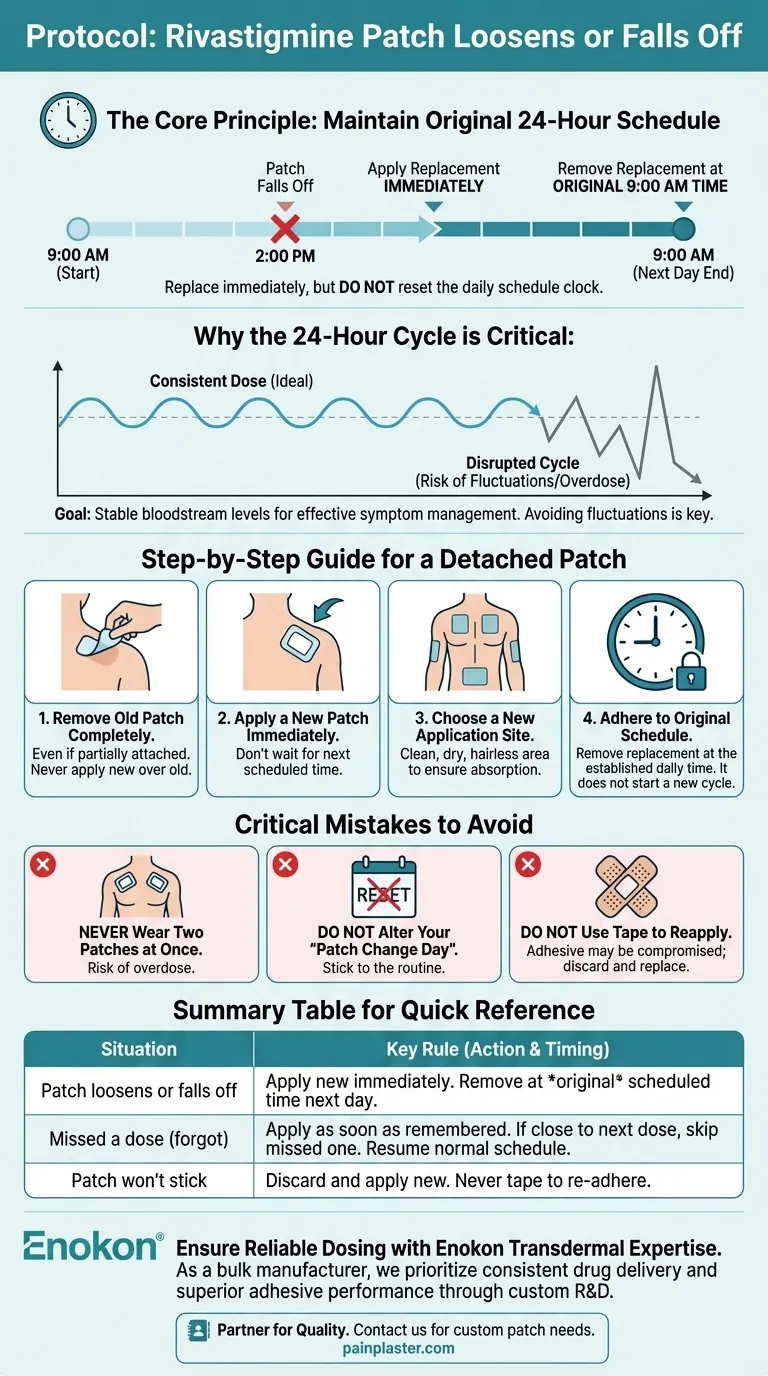
If a rivastigmine patch loosens or falls off, the immediate action is to replace it with a new patch. Critically, you must then remove this new replacement patch at the same time you were scheduled to remove the original one. This ensures the 24-hour dosing schedule remains consistent and prevents an overdose.
The core principle is to maintain the original 24-hour medication cycle without interruption. A detached patch should be replaced immediately, but this does not reset the clock on your daily schedule.

The Goal: A Consistent Therapeutic Dose
Rivastigmine patches are designed to deliver a steady, continuous dose of medication over a 24-hour period. This consistency is essential for managing symptoms effectively.
Why the 24-Hour Cycle is Critical
Maintaining a stable level of the drug in the bloodstream is the primary goal. Disrupting the 24-hour cycle can lead to fluctuations in medication levels, potentially reducing its therapeutic benefit or increasing side effects.
The Logic of the "Replace and Maintain" Rule
When a patch falls off, the drug delivery stops. Applying a new one restores it. By removing the replacement patch at the original scheduled time, you ensure the patient receives medication for as much of the 24-hour period as possible without creating a double dose on the following day.
A Step-by-Step Guide for a Detached Patch
Follow this precise sequence if a patch becomes loose or falls off completely.
1. Remove the Old Patch
If the patch is still partially attached, remove it completely. Never attempt to apply a new patch while the old one is still on the skin, even if it's loose.
2. Apply a New Patch Immediately
Apply a fresh patch as soon as you notice the original one is gone. Do not wait until the next scheduled application time.
3. Choose a New Application Site
Always apply the new patch to a different, clean, dry, and hairless area of skin. This prevents skin irritation and ensures proper absorption. Good locations include the upper or lower back, upper arm, or chest.
4. Adhere to the Original Schedule
This is the most important step. If your normal time to change the patch is 9:00 AM, you must remove the replacement patch at 9:00 AM the next day and apply the next scheduled patch. The replacement does not start a new 24-hour cycle.
Critical Mistakes to Avoid
Managing this situation correctly is just as much about what you don't do. These errors can compromise patient safety and treatment efficacy.
Never Wear Two Patches at Once
Applying an extra patch to "make up" for a lost one can lead to an overdose. The body should only ever have one rivastigmine patch on it at any given time.
Do Not Alter Your "Patch Change Day"
Resist the temptation to restart the 24-hour clock when you apply a replacement. Sticking to the established daily routine is paramount for long-term treatment success.
Do Not Use Tape to Reapply
If a patch does not stick, do not use bandages or tape to hold it in place. Discard it and apply a new patch, as its adhesive and drug-delivery system may be compromised.
Making the Right Choice for Patient Safety
Your response to a detached patch should always prioritize safety and consistency.
- If a patch falls off: Replace it immediately with a new one, but remove it at the originally scheduled time the next day.
- If you miss a dose entirely (forget to apply a patch): Apply a patch as soon as you remember, but maintain the original removal time. If it's almost time for the next scheduled patch, skip the missed one and continue with the regular schedule.
- If you are ever unsure: Contact your pharmacist or prescribing doctor immediately for guidance specific to the patient's situation.
Ultimately, your goal is to ensure the patient receives a safe and consistent dose of their medication every day.
Summary Table:
| Situation | Action | Key Rule |
|---|---|---|
| Patch loosens or falls off | Apply a new patch immediately. | Remove the replacement patch at the original scheduled time the next day. |
| Missed a dose (forgot to apply) | Apply a patch as soon as remembered. | If it's almost time for the next dose, skip the missed one and resume the normal schedule. |
| Patch won't stick | Discard it and apply a new one. | Never use tape or a bandage to re-adhere a patch. |
Ensure Reliable Dosing with Quality Transdermal Patches
Managing medication through patches requires absolute reliability. As Enokon, a bulk manufacturer of transdermal patches and pain plasters, we understand that consistent drug delivery is critical for patient safety and treatment efficacy. Our technical expertise ensures superior adhesive performance and precise, controlled release of medication.
Are you a healthcare distributor or pharma brand seeking a reliable manufacturing partner?
We specialize in custom R&D and development to create patches that stay on and deliver the correct dose, every time. Benefit from our expertise to enhance your product line and ensure patient well-being.
Contact our experts today to discuss your custom transdermal patch needs.
Visual Guide
Related Products
- Herbal Eye Protection Patch Eye Patch
- Far Infrared Deep Heat Relief Patches Medicated Pain Relief Patches
- Asthma Cough and Pain Relief Patch for Adults and Kids
- Menthol Gel Pain Relief Patch
- Icy Hot Menthol Medicine Pain Relief Patch
People Also Ask
- When should a doctor be consulted regarding the use of this patch? Key Safety Guidelines
- What are the main benefits of using eye patches in a skincare routine? Revitalize Your Under-Eye Area
- Should under eye patches be applied before or after moisturizer? Optimize Your Skincare Routine
- What factors should be considered when purchasing eye patches? Essential Guide for Safe & Effective Use
- How can using eye patches contribute to a self-care skincare routine? Boost Hydration & Relaxation















