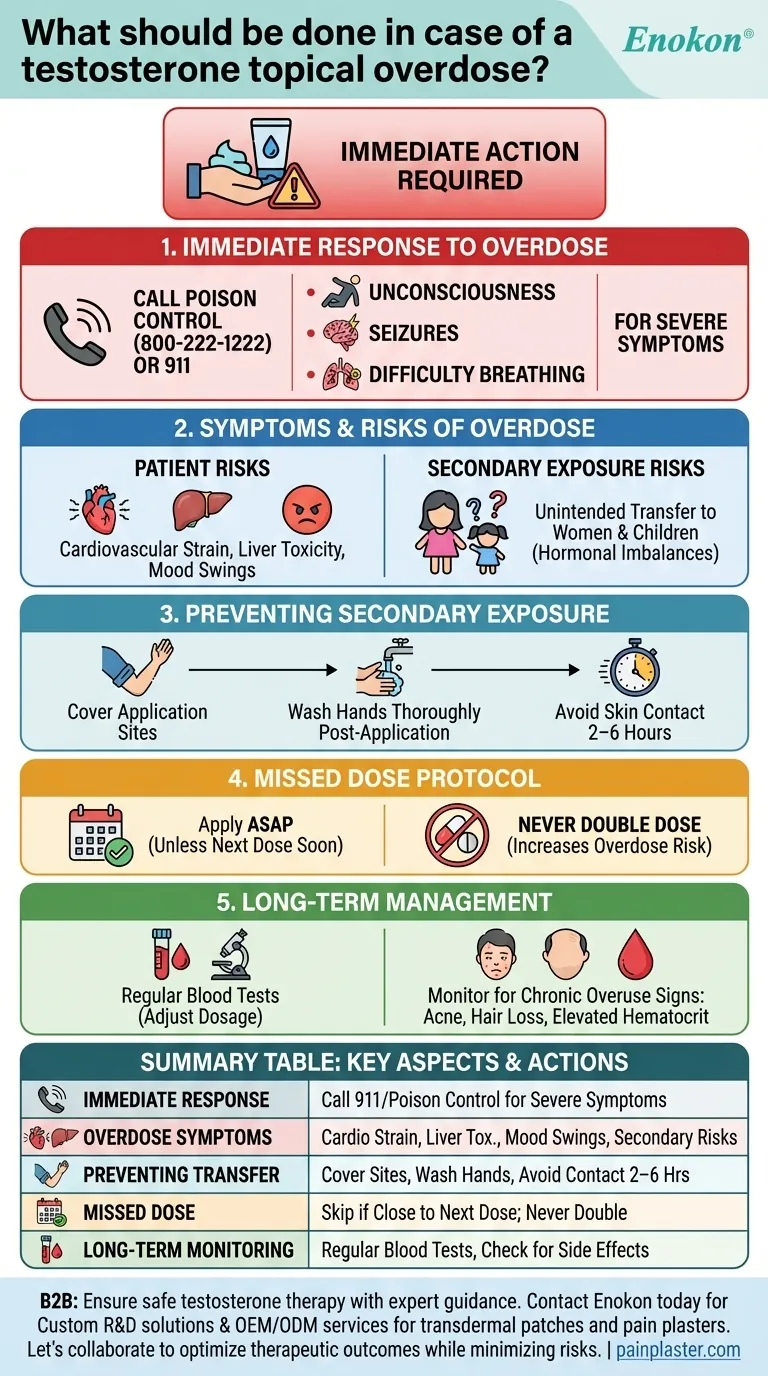
Testosterone topical overdose requires immediate action to mitigate potential health risks. The primary steps involve contacting poison control or emergency services, especially if severe symptoms like seizures, difficulty breathing, or unconsciousness occur. Overdose can result from applying excessive amounts or prolonged use of patches, gels, or creams. Secondary exposure is also a concern, as testosterone can transfer to others through skin contact, particularly affecting women and children. Proper application hygiene, such as covering the treated area and washing hands, helps prevent accidental transfer. If a dose is missed, it should not be doubled; instead, the regular schedule should resume.

Key Points Explained:
-
Immediate Response to Overdose
- Contact poison control (e.g., 800-222-1222 in the U.S.) or emergency services (911) if severe symptoms arise, including:
- Collapse or unconsciousness
- Seizures
- Difficulty breathing
- Overdose may occur from applying too much product or leaving patches on for extended periods.
- Contact poison control (e.g., 800-222-1222 in the U.S.) or emergency services (911) if severe symptoms arise, including:
-
Symptoms and Risks of Overdose
- Excessive testosterone absorption can lead to:
- Cardiovascular strain
- Liver toxicity
- Aggressive behavior or mood swings
- Secondary exposure risks include unintended transfer to others, particularly women and children, causing hormonal imbalances or developmental issues.
- Excessive testosterone absorption can lead to:
-
Preventing Secondary Exposure
- Cover application sites with clothing after applying topical testosterone.
- Wash hands thoroughly post-application.
- Avoid skin-to-skin contact until the product is fully absorbed (e.g., 2–6 hours for gels).
-
Missed Dose Protocol
- If a dose is missed, apply it as soon as remembered—unless the next dose is due soon.
- Never double the dose to compensate, as this increases overdose risk.
-
Long-Term Management
- Monitor for signs of chronic overuse (e.g., acne, hair loss, elevated hematocrit).
- Regular blood tests can help adjust dosage to safe levels.
Have you considered how subtle changes in application habits might accumulate into overdose risks over time? These protocols highlight the balance between therapeutic benefits and the vigilance needed to avoid harm—a reminder of how precision matters in hormone therapies.
Summary Table:
| Key Aspect | Action/Consideration |
|---|---|
| Immediate Response | Call poison control (800-222-1222) or 911 for severe symptoms (seizures, unconsciousness). |
| Overdose Symptoms | Cardiovascular strain, liver toxicity, mood swings, or secondary exposure risks. |
| Preventing Transfer | Cover application sites, wash hands, avoid skin contact for 2–6 hours post-application. |
| Missed Dose | Skip if close to next dose; never double apply. |
| Long-Term Monitoring | Regular blood tests to adjust dosage and check for acne, hair loss, or hematocrit spikes. |
Ensure safe testosterone therapy with expert guidance
If you or your patients need support with hormone therapy protocols, contact Enokon today. As a trusted bulk manufacturer of transdermal patches and pain plasters, we provide:
- Custom R&D solutions for precise dosing and application safety.
-
OEM/ODM services tailored to healthcare brands and distributors.
Let’s collaborate to optimize therapeutic outcomes while minimizing risks.
Visual Guide
Related Products
- Prostate Pain Kidney Health Care Patch for Men
- Capsaicin Chili Medicated Pain Relief Patches
- Heating Pain Relief Patches for Menstrual Cramps
- Mugwort Wormwood Pain Relief Patch for Neck Pain
- Detox Foot Patches for Detoxification
People Also Ask
- What should be done before undergoing an MRI while using testosterone patches? Remove it to prevent serious burns.
- What should be done if a dose of testosterone patches is missed? Regain Stability and Safety
- What should be done if a testosterone patch is missed or falls off? Follow these simple timing rules for safety and consistency.
- What should patients tell their doctor before using testosterone patches? A Guide to Safe Treatment
- What should be done in case of a testosterone patch overdose? A Step-by-Step Emergency Guide