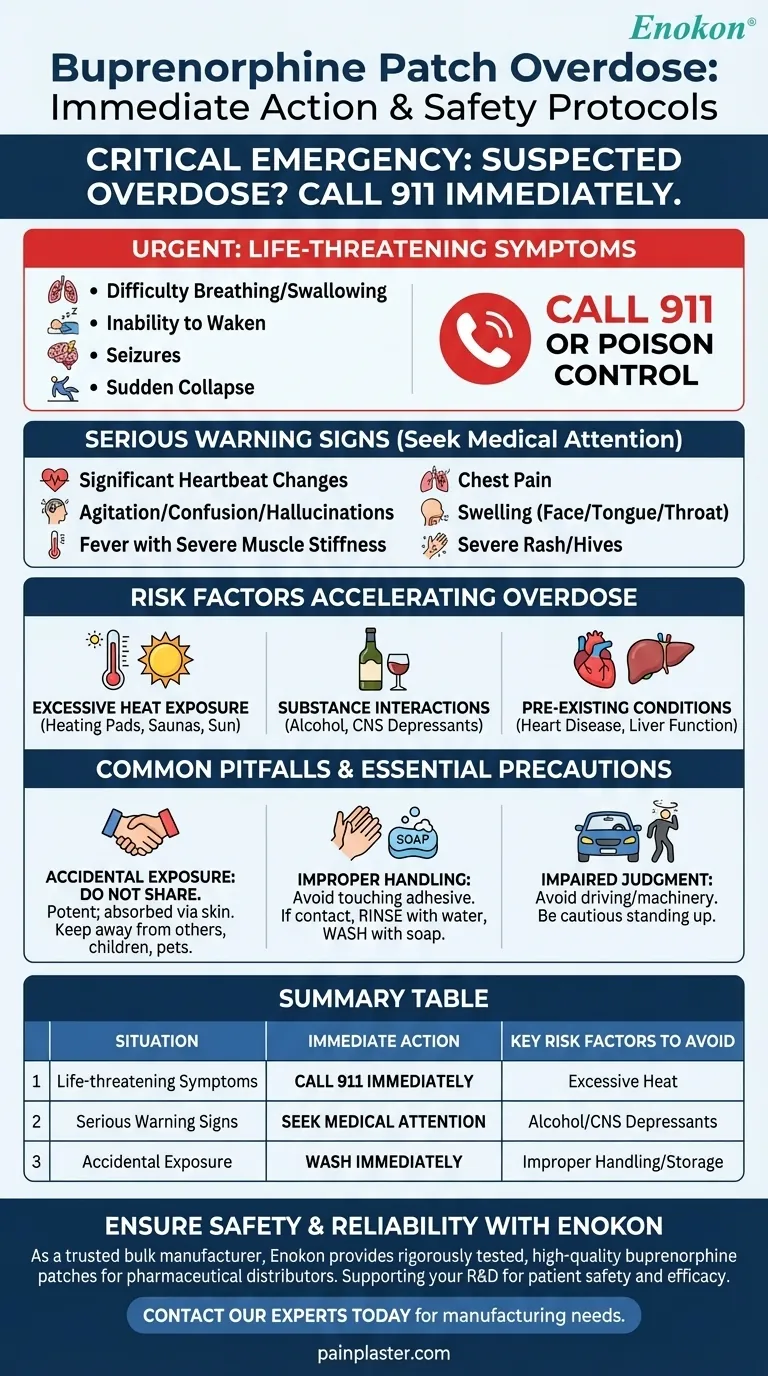
In the event of a suspected buprenorphine patch overdose, you must take immediate action. If the person has collapsed, is having a seizure, has trouble breathing, or cannot be awakened, call 911 or your local poison control helpline for emergency medical attention without delay. These are signs of a life-threatening medical emergency that requires professional intervention.
A buprenorphine patch overdose is a critical medical event where the primary response is to seek immediate emergency help. Preventing an overdose hinges on understanding the risk factors, recognizing the warning signs, and adhering to strict safety protocols for handling the medication.

Recognizing the Signs of an Overdose
Distinguishing between common side effects and a true overdose is crucial. An overdose occurs when the body is overwhelmed by the amount of medication released.
Critical Emergency Symptoms
The most severe symptoms require an immediate 911 call. Do not wait to see if they improve.
These include:
- Difficulty breathing or swallowing
- Inability to be awakened
- Seizures
- Sudden collapse
Other Serious Warning Signs
Other serious reactions may indicate a dangerous level of medication in the body. Seek medical attention right away if you observe any of the following:
- Significant changes in heartbeat
- Agitation, confusion, or hallucinations
- Fever with severe muscle stiffness
- Chest pain
- Swelling of the face, tongue, or throat
- A severe rash or hives
Factors That Increase Overdose Risk
An overdose is not always caused by incorrect application. Several external factors can dangerously accelerate the rate at which the medication enters your bloodstream.
Exposure to Excessive Heat
Avoid sources of excessive heat while wearing the patch, such as heating pads, electric blankets, saunas, or prolonged direct sun exposure. Heat can cause the patch to release the medication much faster than intended, leading to a sudden and dangerous spike in dosage.
Interactions with Other Substances
Combining buprenorphine with alcohol or other central nervous system depressants, including "street drugs," can severely amplify its effects. This dramatically increases the risk of respiratory depression, where breathing becomes dangerously slow and shallow.
Pre-existing Medical Conditions
Your personal health history is a critical factor. Conditions like heart disease, a history of seizures, or impaired liver function can alter how your body processes the medication, making you more susceptible to adverse effects. Always provide your doctor with a complete medical history.
Common Pitfalls and Essential Precautions
Safe use of a transdermal patch goes beyond simply applying it. Adhering to strict handling and awareness protocols is non-negotiable for preventing accidental overdose or exposure.
Accidental Exposure
The medication is potent and can be absorbed through the skin by anyone who handles it. Do not let anyone else use your patches. Selling or giving away this medication is illegal and can cause severe harm or death.
Improper Handling
When opening the pouch, be careful not to tear the patch itself. Avoid touching the adhesive side with your fingers. If you do make contact, immediately rinse the area with a large amount of water and then wash thoroughly with soap.
Impaired Judgment and Coordination
Buprenorphine can cause dizziness and impair your ability to think clearly. Do not drive a car or operate heavy machinery until you are certain how the medication affects you. Be particularly cautious when standing up from a sitting or lying position to avoid falls.
Making the Right Choice for Your Goal
Your approach to using this medication must be guided by a clear understanding of your role and responsibilities.
- If your primary focus is personal safety as a patient: Adhere strictly to your doctor's instructions, be vigilant about avoiding heat sources, and never combine this medication with alcohol.
- If your primary focus is caring for someone using the patch: Memorize the signs of an overdose and be prepared to call for emergency help immediately if you witness them.
- If your primary focus is preventing accidental exposure: Ensure the patch is stored securely out of reach of children and pets, and always wash your hands after handling the medication.
Ultimately, proactive awareness and strict adherence to safety guidelines are the most effective tools for using this medication safely and effectively.
Summary Table:
| Situation | Immediate Action | Key Risk Factors to Avoid |
|---|---|---|
| Life-threatening symptoms (e.g., difficulty breathing, seizures, unresponsiveness) | Call 911 or your local emergency number immediately. | Exposure to excessive heat (heating pads, saunas, hot baths). |
| Serious warning signs (e.g., chest pain, severe rash, agitation) | Seek immediate medical attention. | Interactions with alcohol or other CNS depressants. |
| Accidental exposure (touching the adhesive gel) | Wash the area immediately with plenty of water and soap. | Improper handling or storage, increasing risk to others. |
Ensure the highest standards of safety and reliability for your transdermal products. As a trusted bulk manufacturer, Enokon provides pharmaceutical distributors and brands with rigorously tested, high-quality buprenorphine patches and custom pain plasters. Our technical expertise supports your custom R&D and product development, ensuring patient safety and medication efficacy. Contact our experts today to discuss your manufacturing needs and how we can partner to deliver safe, effective transdermal solutions.
Visual Guide
Related Products
- Far Infrared Deep Heat Relief Patches Medicated Pain Relief Patches
- Far Infrared Knee Pain Patch Heat Patches for Pain Relief
- Far Infrared Pain Patch Relief Pain Reliever for Back
- Far Infrared Heat Pain Relief Patches Transdermal Patches
- Asthma Cough and Pain Relief Patch for Adults and Kids
People Also Ask
- How do pain relief patches provide targeted relief? Discover the Science Behind Effective Pain Management
- How effective are pain relief patches for muscle pain? Target Localized Pain with Transdermal Delivery
- What are pain relief patches and how are they used? A Guide to Safe, Targeted Relief
- How do pain relief patches compare to other pain relief methods? Discover Targeted, Long-Lasting Relief
- How do Deep Heat Pain Relief Patches provide pain relief? Discover the Drug-Free Mechanism
















