For breastfeeding mothers, using estradiol transdermal medication requires careful consideration and a clear understanding of its potential effects. The primary concern is that the hormone, absorbed through your skin, may alter your milk production or its composition. While it may be prescribed when no alternative is suitable, this decision necessitates vigilant monitoring of your infant.
The core issue with transdermal estradiol during breastfeeding is not significant hormone transfer to the infant, but its potential to suppress your milk supply. Therefore, the focus must be on ensuring your baby continues to get enough milk.

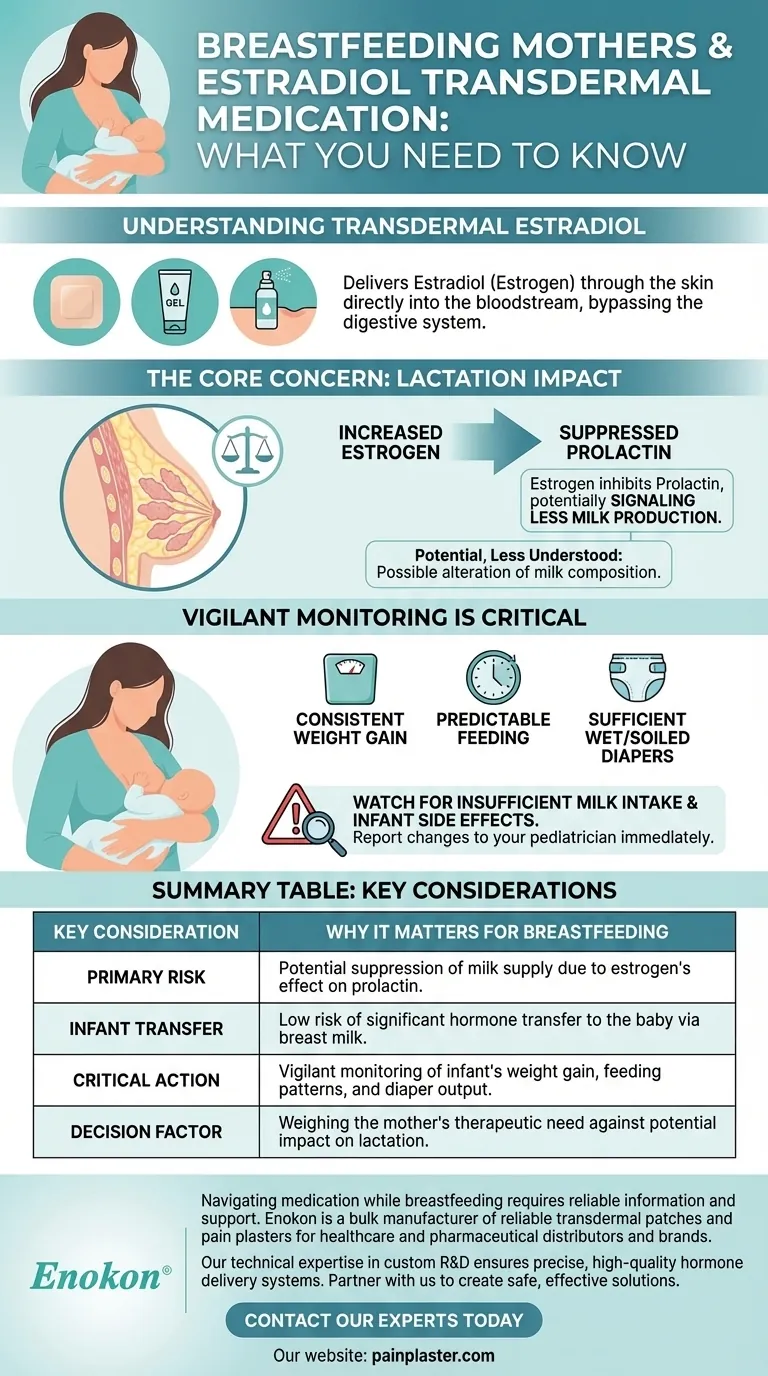
How Transdermal Estradiol Works
Estradiol is a form of estrogen, a primary female sex hormone. Transdermal application is a method used to deliver this hormone into your bloodstream steadily.
Administration Through the Skin
This medication comes in several forms, including a patch, gel, or spray. When applied, the estradiol is absorbed directly through the skin and enters your circulation, bypassing the digestive system.
The Goal of Hormone Therapy
This therapy is typically used to supplement the body's natural estrogen levels, often to manage symptoms associated with menopause or other conditions causing low estrogen.
The Core Concern: Impact on Lactation
The introduction of external estrogens like estradiol can interfere with the delicate hormonal balance required for breastfeeding.
Potential Effect on Milk Production
Lactation is driven primarily by the hormone prolactin. Estrogen has an inhibitory effect on prolactin, meaning higher estrogen levels can signal your body to produce less milk. This is the most significant potential issue.
Potential Changes to Milk Composition
While less understood, there is a possibility that estradiol could also alter the nutritional or hormonal makeup of your breast milk.
Understanding the Trade-offs
When considering this medication, it is crucial to weigh the therapeutic benefits for the mother against the potential impacts on the nursing infant. Your healthcare provider is your essential partner in this assessment.
Monitoring for Insufficient Milk Intake
The most critical task is to watch for signs that your baby is not getting enough milk. This is more important than theoretical concerns about the hormone itself.
Key signs of adequate intake include consistent weight gain, predictable feeding patterns, and a sufficient number of wet and soiled diapers each day.
Observing for Infant Side Effects
You should also observe your infant for any unusual changes in behavior or health. If you notice any new or concerning symptoms after starting the medication, report them to your pediatrician and prescribing doctor immediately.
Making an Informed Decision with Your Doctor
The choice to use transdermal estradiol while breastfeeding is a medical decision that balances your health needs with the well-being of your child.
- If your medical need for estradiol is urgent: Your primary focus should be on diligent, daily monitoring of your infant's weight gain and your own milk supply.
- If you have flexibility in your treatment: Discuss all alternative medications, including non-hormonal options, with your healthcare provider to see if a different approach can meet your needs.
Ultimately, working closely with your medical team is the key to safely managing your health while ensuring your baby continues to thrive.
Summary Table:
| Key Consideration | Why It Matters for Breastfeeding |
|---|---|
| Primary Risk | Potential suppression of milk supply due to estrogen's effect on prolactin. |
| Infant Transfer | Low risk of significant hormone transfer to the baby via breast milk. |
| Critical Action | Vigilant monitoring of infant's weight gain, feeding patterns, and diaper output. |
| Decision Factor | Weighing the mother's therapeutic need against potential impact on lactation. |
Navigating medication while breastfeeding requires reliable information and support. At Enokon, we are a bulk manufacturer of reliable transdermal patches and pain plasters for healthcare and pharmaceutical distributors and brands. Our technical expertise in custom R&D and development ensures precise, high-quality hormone delivery systems. If your organization is developing or distributing transdermal therapies for patients like breastfeeding mothers, partner with us to create safe, effective solutions. Contact our experts today to discuss your project needs.
Visual Guide
Related Products
- Far Infrared Heat Pain Relief Patches Transdermal Patches
- Far Infrared Deep Heat Relief Patches Medicated Pain Relief Patches
- Capsaicin Chili Medicated Pain Relief Patches
- Heating Pain Relief Patches for Menstrual Cramps
- Far Infrared Pain Patch Relief Pain Reliever for Back
People Also Ask
- What are the key features of the Deep Heat Pain Relief Back Patch? Get Up to 16 Hours of Drug-Free Relief
- How do Deep Heat Pain Relief Patches provide pain relief? Discover the Drug-Free Mechanism
- What types of pain can the Deep Heat Pain Relief Back Patch be used for? Targeted Relief for Muscles & Joints
- What did the UK Million Women Study find regarding transdermal versus oral hormone therapy? A Safer Choice for Gallbladder Health
- How does capsaicin work in the medicated heat patch? The Science Behind Pain Relief














