When you stop using the birth control patch, your body begins to transition away from the steady supply of synthetic hormones and back to its own natural hormonal rhythm. This adjustment period is temporary and can bring noticeable changes, most critically an immediate return to fertility, along with potential shifts in your menstrual cycle and skin.
The core takeaway is that your body will return to its pre-patch state. Fertility can return immediately, while your menstrual cycle may take one to three months to regulate, and any symptoms the patch was masking, like acne or heavy periods, may reappear.

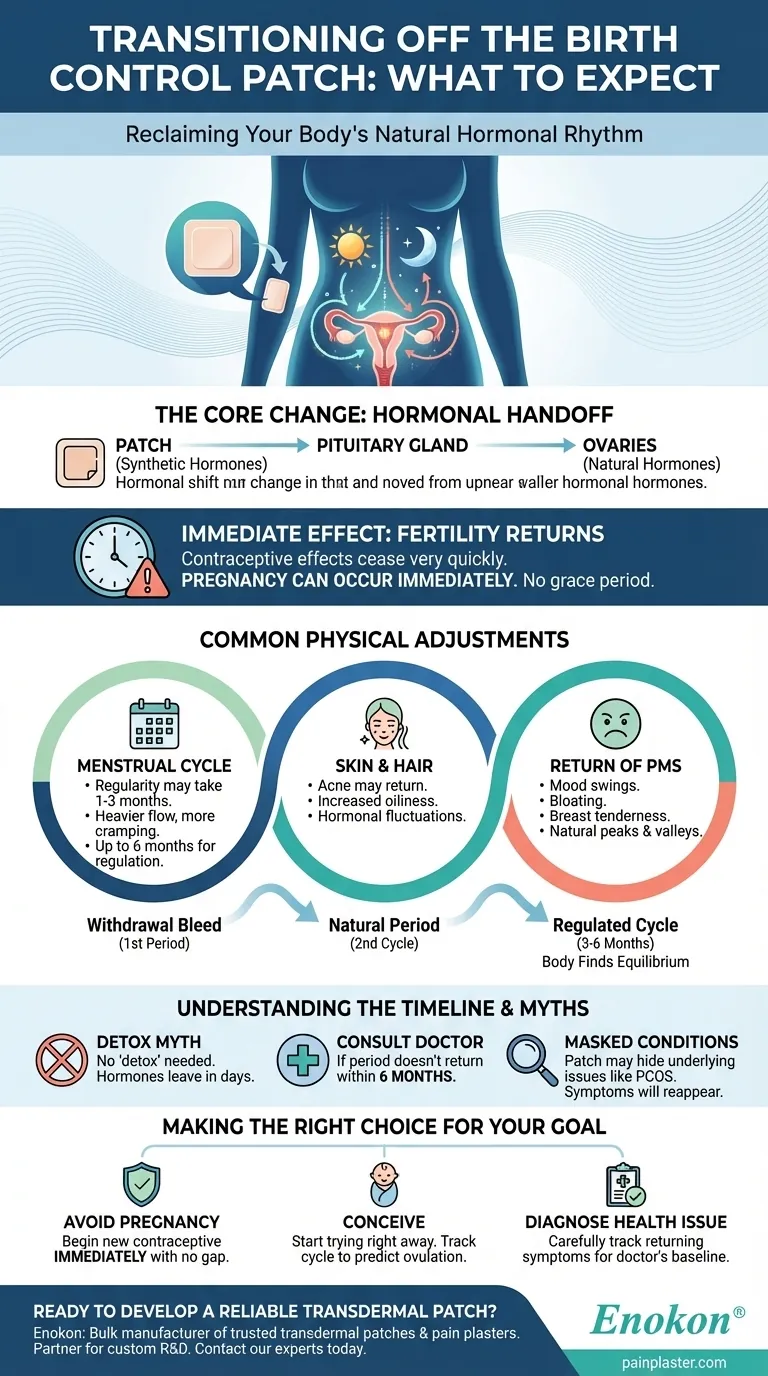
The Core Change: Reclaiming Your Natural Hormonal Rhythm
Stopping the birth control patch signals your body to restart its own production and regulation of the hormones that drive the menstrual cycle. The changes you experience are a direct result of this hormonal handoff.
Why This Transition Happens
The birth control patch releases a consistent dose of synthetic estrogen and progestin. These hormones prevent ovulation, thicken cervical mucus, and thin the uterine lining to prevent pregnancy. When you remove that external source, your brain's pituitary gland resumes its job of signaling the ovaries to mature and release an egg.
The Most Immediate Effect: Return of Fertility
The most critical factor to understand is that your fertility can return almost immediately. The contraceptive effects of the patch cease very quickly after you stop using it. You should not assume there is a grace period where you are protected from pregnancy.
Common Physical Adjustments to Expect
As your body finds its new equilibrium, you may notice several temporary changes. These often reflect what your cycle and body were like before you started using the patch.
Changes to Your Menstrual Cycle
Your first period after stopping the patch is a "withdrawal bleed," but subsequent cycles are your body's natural period. It can take one to two months for your regular cycle to return, though for some, especially those with previously irregular periods, it could take up to six months. Your periods may become heavier, less regular, and you might experience more cramping than you did on the patch.
Skin and Hair Changes
If the patch helped control your acne, you might see breakouts return. The steady, controlled hormone levels from the patch can suppress the androgen activity that contributes to acne. As your natural, fluctuating hormones return, so can acne.
Return of Pre-Menstrual Symptoms (PMS)
Hormonal birth control often smooths out the hormonal peaks and valleys that can cause PMS symptoms like mood swings, bloating, or breast tenderness. As your natural cycle resumes, these symptoms may return.
Understanding the Trade-offs and Timeline
Managing the transition is about understanding the timeline and being prepared for the changes. The process is straightforward, but being aware of the potential pitfalls is key.
The Myth of a "Detox" Period
Your body does not need to "detox" from the hormones. They leave your system within days, which is why fertility returns so quickly. The adjustment period is simply your body re-establishing its own cyclical rhythm.
Masked Underlying Conditions
The patch can mask symptoms of underlying conditions like Polycystic Ovary Syndrome (PCOS) or endometriosis. If you had very irregular periods, severe acne, or debilitating cramps before starting the patch, these symptoms will likely return and may warrant a discussion with your healthcare provider.
When to Consult a Doctor
While an adjustment period is normal, you should speak with a doctor if your period has not returned within six months of stopping the patch. This could indicate an underlying issue that the patch was previously managing.
Making the Right Choice for Your Goal
Navigating this transition effectively depends entirely on your reason for stopping the patch. Your next steps should be guided by your personal health goals.
- If your primary focus is to avoid pregnancy: You must begin using a new contraceptive method immediately, with no gap in coverage.
- If your primary focus is to conceive: You can start trying right away, but tracking your cycle for a few months can help you more accurately predict ovulation.
- If your primary focus is to diagnose a health issue: Carefully track any returning symptoms like acne, cramps, or cycle irregularity to give your doctor the clearest possible picture of your body's natural baseline.
Ultimately, stopping the birth control patch is a safe process that allows you to reconnect with your body's unique and natural rhythm.
Summary Table:
| Change | What to Expect | Timeline |
|---|---|---|
| Fertility | Can return immediately; contraceptive protection ends. | Within days |
| Menstrual Cycle | Periods may become heavier, irregular; may experience cramping. | Regulates in 1-3 months (can take up to 6) |
| Skin & PMS | Acne may return; pre-menstrual symptoms like mood swings may reappear. | Varies; often within 1-2 cycles |
Ready to develop a reliable, comfortable transdermal patch for your patients? As Enokon, a bulk manufacturer of trusted transdermal patches and pain plasters, we partner with healthcare and pharma distributors and brands. Benefit from our technical expertise for custom R&D and development to create a product that meets your specific needs. Contact our experts today to discuss your project.
Visual Guide
Related Products
- Prostate Pain Kidney Health Care Patch for Men
- Menthol Gel Pain Relief Patch
- Capsaicin Chili Medicated Pain Relief Patches
- Lidocaine Hydrogel Pain Relief Patch for Pain Relief
- Far Infrared Deep Heat Relief Patches Medicated Pain Relief Patches
People Also Ask
- What should patients tell their doctor before using testosterone patches? A Guide to Safe Treatment
- How often should testosterone patches be applied? Daily Dosage & Best Practices
- What should be done if a dose of testosterone patches is missed? Regain Stability and Safety
- What precautions should be taken when applying testosterone patches? Maximize Safety and Effectiveness
- What should be done if a testosterone patch is missed or falls off? Follow these simple timing rules for safety and consistency.















