While no specific dosage adjustments are defined for elderly patients, the use of buprenorphine patches requires significantly heightened caution. This population often has increased sensitivity to opioids and a higher likelihood of co-existing medical conditions, making careful monitoring and strict adherence to safety protocols absolutely essential for managing chronic pain effectively.
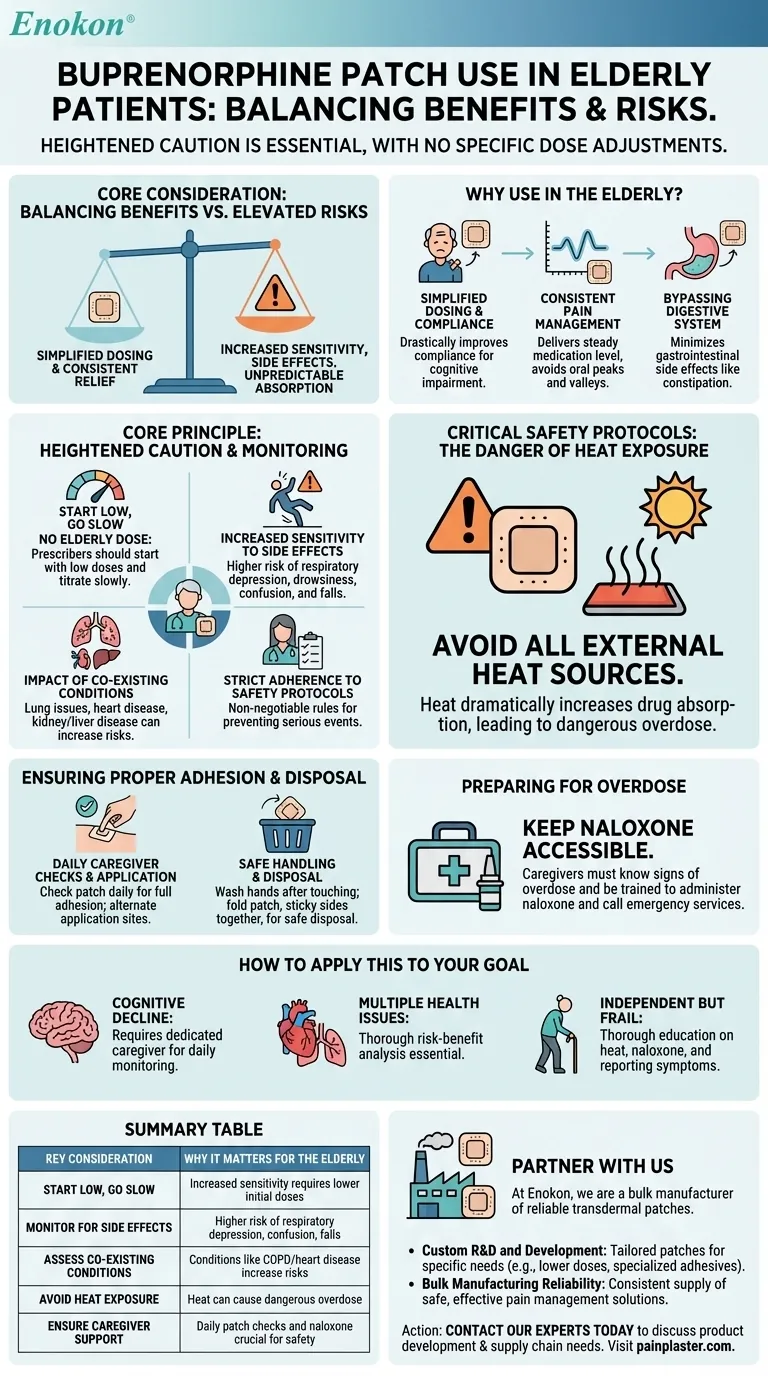
The core consideration is balancing the patch's benefits—such as simplified dosing and steady pain relief—against the elevated risks in the elderly, including increased sensitivity to side effects, unpredictable drug absorption, and the potential for severe complications from underlying health issues.

Why Buprenorphine Patches Are Used in the Elderly
While the risks are higher, transdermal patches offer distinct advantages for managing chronic pain in an older population, which is why they are often considered.
Simplified Dosing and Compliance
For patients with cognitive impairment, such as Alzheimer's or Parkinson's disease, a patch that is applied once every few days drastically improves compliance over a complex pill schedule.
Consistent Pain Management
The patch delivers a steady, continuous level of medication. This avoids the peaks and valleys of oral medication, providing more consistent and predictable pain relief around the clock.
Bypassing the Digestive System
Oral opioids can cause significant gastrointestinal issues like constipation, which can be particularly problematic for older adults. A transdermal patch bypasses the stomach and intestines, minimizing these side effects.
The Core Principle: Heightened Caution and Monitoring
The official guidance to use "caution" without specific dose adjustments means that treatment must be highly individualized and closely supervised by a healthcare provider.
The Meaning of "No Elderly Dose"
The lack of a specific dose for this population means prescribers should always start low and go slow. An elderly patient may experience significant pain relief and side effects from a dose that a younger patient would barely feel.
Increased Sensitivity to Side Effects
Older adults are more susceptible to the central nervous system effects of buprenorphine. This includes a higher risk of respiratory depression (slowed or stopped breathing), severe drowsiness, confusion, and dizziness, which can directly lead to falls and injury.
The Impact of Co-existing Conditions
Many elderly patients have pre-existing conditions that can be dangerously exacerbated by buprenorphine. It is critical to inform the provider about any history of:
- Lung or breathing problems (like COPD)
- Heart disease or irregular heartbeat
- Liver or kidney disease
- History of head injury or seizures
- Low adrenal function
Understanding the Trade-offs and Critical Safety Protocols
Safe use of the buprenorphine patch in an elderly patient depends on strict adherence to a set of non-negotiable safety rules. These are not suggestions; they are requirements for preventing a serious adverse event.
The Danger of Heat Exposure
Avoid all external heat sources on or near the patch, such as heating pads, hot tubs, saunas, or even prolonged direct sun exposure. Heat dramatically increases the rate of drug absorption through the skin, which can quickly lead to a dangerous overdose.
Ensuring Proper Adhesion and Application
A caregiver should check the patch daily to ensure it is fully and properly adhered to the skin. If a patch falls off, a new one should be applied to a completely different application site. Always alternate sites with each new patch to prevent skin irritation.
Safe Handling and Disposal
Always wash your hands after touching a buprenorphine patch. To dispose of a used patch, fold it in half with the sticky sides together and return it to a pharmacy if possible, or follow specific disposal instructions from your provider. This prevents accidental exposure to children, pets, or other caregivers.
Preparing for a Potential Overdose
A prescription for naloxone should be obtained and kept readily accessible. Caregivers and family members must know the signs of an overdose (extreme drowsiness, unresponsiveness, slow or shallow breathing) and be trained on how to administer naloxone. Always call emergency services immediately after giving naloxone.
How to Apply This to Your Goal
The decision to use a buprenorphine patch requires a clear-eyed assessment of the patient's specific circumstances and support system.
- If your primary focus is managing pain in a patient with cognitive decline: The patch offers a major compliance advantage but requires a dedicated caregiver for daily monitoring of patch adhesion, side effects, and signs of overdose.
- If the patient has multiple health issues (especially heart or lung disease): The risks are significantly higher, and a thorough risk-benefit analysis with the provider is essential before starting or continuing treatment.
- If the patient is independent but frail: They must be thoroughly educated on the critical risks of heat exposure, the importance of having naloxone, and the need to immediately report any new symptoms like excessive dizziness or confusion.
Ultimately, safe and effective pain management with buprenorphine patches in the elderly depends on a collaborative partnership between the patient, their caregivers, and their healthcare team.
Summary Table:
| Key Consideration | Why It Matters for the Elderly |
|---|---|
| Start Low, Go Slow | Increased sensitivity to opioids requires lower initial doses and careful titration. |
| Monitor for Side Effects | Higher risk of respiratory depression, confusion, dizziness, and falls. |
| Assess Co-existing Conditions | Conditions like COPD, heart disease, or kidney issues can increase risks. |
| Avoid Heat Exposure | Heat can cause a dangerous overdose by increasing drug absorption. |
| Ensure Caregiver Support | Daily patch checks and naloxone availability are crucial for safety. |
Need a reliable transdermal patch solution for your patients?
At Enokon, we are a bulk manufacturer of reliable transdermal patches and pain plasters, including formulations for sensitive populations. We partner with healthcare distributors and pharmaceutical brands to deliver high-quality, consistent products.
Partner with us to benefit from:
- Custom R&D and Development: Our technical expertise allows us to develop patches tailored to specific patient needs, such as those requiring lower doses or specialized adhesives for fragile skin.
- Bulk Manufacturing Reliability: Ensure a consistent supply of safe and effective pain management solutions for your customers.
Contact our experts today to discuss how we can support your product development and supply chain needs.
Visual Guide
Related Products
- Far Infrared Deep Heat Relief Patches Medicated Pain Relief Patches
- Far Infrared Heat Pain Relief Patches Transdermal Patches
- Mugwort Wormwood Pain Relief Patch for Neck Pain
- Menthol Gel Pain Relief Patch
- Icy Hot Menthol Medicine Pain Relief Patch
People Also Ask
- What are pain relief patches and how are they used? A Guide to Safe, Targeted Relief
- How often should pain relief patches be used? Get the Right Schedule for Targeted Relief
- How do pain relief patches work? A Guide to Targeted, Long-Lasting Pain Relief
- How do pain relief patches compare to other pain relief methods? Discover Targeted, Long-Lasting Relief
- How quickly does the Deep Heat Pain Relief Back Patch activate and how long does it provide warmth? Get 16-Hour Relief














