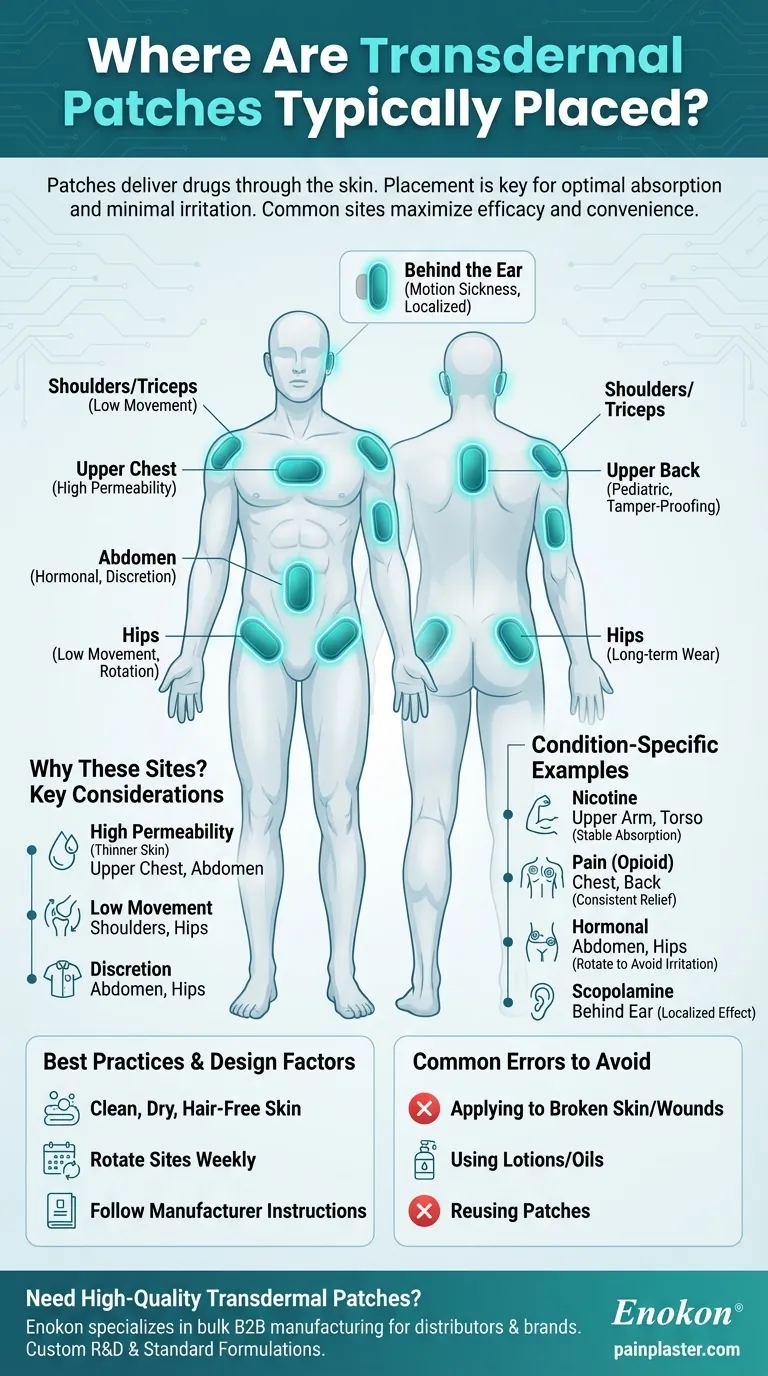
Transdermal patches are designed for systemic drug delivery through the skin, with placement locations carefully selected to optimize absorption and minimize irritation. The most common application sites include the upper chest, shoulders/triceps, abdomen, and hips, chosen based on factors like skin permeability, convenience, and the specific medication's requirements. Proper application involves clean, dry, hair-free skin with regular site rotation to prevent skin irritation. These patches treat diverse conditions from nicotine addiction to chronic pain, leveraging multi-layer technology for controlled drug release.

Key Points Explained:
-
Primary Application Sites
Transdermal patches are typically applied to areas with:- High permeability: Upper chest and abdomen have thinner skin and good blood flow.
- Low movement: Shoulders/triceps and hips reduce friction-induced detachment.
- Discretion: Easily concealed under clothing (e.g., abdomen or hip for hormonal patches).
-
Condition-Specific Placement
- Nicotine patches: Often placed on upper arms or torso to stabilize absorption rates.
- Opioid patches (fentanyl): Applied to chest/back for consistent pain relief.
- Hormonal patches (estrogen/testosterone): Rotated between abdomen/hips to avoid skin irritation.
- Scopolamine (motion sickness): Placed behind the ear for localized effect.
-
Anatomical Considerations
- Skin preparation: Clean, dry, and hair-free skin ensures adhesion and absorption. Shaving is preferred over clipping to avoid microcuts.
- Rotation protocol: Alternating sites (e.g., left/right hip weekly) prevents skin breakdown or reduced drug efficacy.
-
Patch Design & Placement Relationship
The multilayer structure (backing, drug reservoir, adhesive) influences placement:- Adhesive strength: Areas with minimal stretching (e.g., upper arm) suit patches needing prolonged wear.
- Drug release rate: Abdominal placement may accelerate absorption due to higher skin temperature.
-
Patient-Specific Adjustments
- Mobility issues: Shoulder placement aids self-application for arthritis patients.
- Pediatric use: Smaller patches may go on the upper back for tamper-proofing.
-
Common Errors to Avoid
- Applying to broken/irritated skin or near wounds.
- Using lotions/oils that degrade adhesive or alter absorption.
- Reusing fallen patches (risk of contamination/dose inconsistency).
-
Emerging Applications
- Microneedle patches: Allow placement on thicker skin areas (e.g., thighs) for vaccines or biologics.
- Wearable sensors: Adhesive tech enables hybrid patches for drug delivery + health monitoring.
For optimal results, always follow manufacturer instructions—placement nuances can affect drug kinetics by up to 30%. Did you know some patches now integrate NFC chips to track adherence? This innovation reflects how a simple application site choice bridges pharmacology and patient lifestyle.
Summary Table:
| Placement Area | Best For | Key Considerations |
|---|---|---|
| Upper Chest | High permeability, good blood flow | Clean, dry skin; rotate sites |
| Shoulders/Triceps | Low movement, discretion | Avoid areas with frequent friction |
| Abdomen | Hormonal patches, convenience | Shave if needed; avoid lotions |
| Hips | Discretion, rotation-friendly | Ideal for long-term wear |
| Behind the Ear | Scopolamine (motion sickness) | Localized effect; small patch size |
Need high-quality transdermal patches tailored to your needs?
At Enokon, we specialize in bulk manufacturing of reliable transdermal patches and pain plasters for healthcare distributors and pharmaceutical brands. Our technical expertise ensures optimal drug delivery, adhesion, and patient comfort. Whether you need standard formulations or custom R&D solutions, we’ve got you covered.
Contact us today to discuss your project and benefit from our industry-leading expertise!
Visual Guide
Related Products
- Far Infrared Heat Pain Relief Patches Transdermal Patches
- Heating Pain Relief Patches for Menstrual Cramps
- Capsaicin Chili Medicated Pain Relief Patches
- Mugwort Wormwood Pain Relief Patch for Neck Pain
- Medical Cooling Gel Patches for Fever Cooling Patches
People Also Ask
- How quickly does the Deep Heat Pain Relief Back Patch activate and how long does it provide warmth? Get 16-Hour Relief
- What are the common side effects of using the medicated heat patch? Understanding Risks & Safe Use
- How do Deep Heat Pain Relief Patches provide pain relief? Discover the Drug-Free Mechanism
- How does capsaicin work in the medicated heat patch? The Science Behind Pain Relief
- What are the key features of the Deep Heat Pain Relief Back Patch? Get Up to 16 Hours of Drug-Free Relief