Anyone prescribed a fentanyl patch should seriously consider having naloxone readily available. While this is a critical precaution for all users, it is especially vital for individuals who live with small children or with anyone who has a history of prescription or street drug abuse. The potent nature of fentanyl means that accidental exposure or misuse can quickly become a life-threatening emergency.
Fentanyl patches carry a significant risk of accidental overdose, not just for the patient but for anyone in the household. Having naloxone is a crucial safety measure that can reverse the effects of an opioid overdose, buying critical time until emergency medical help arrives.

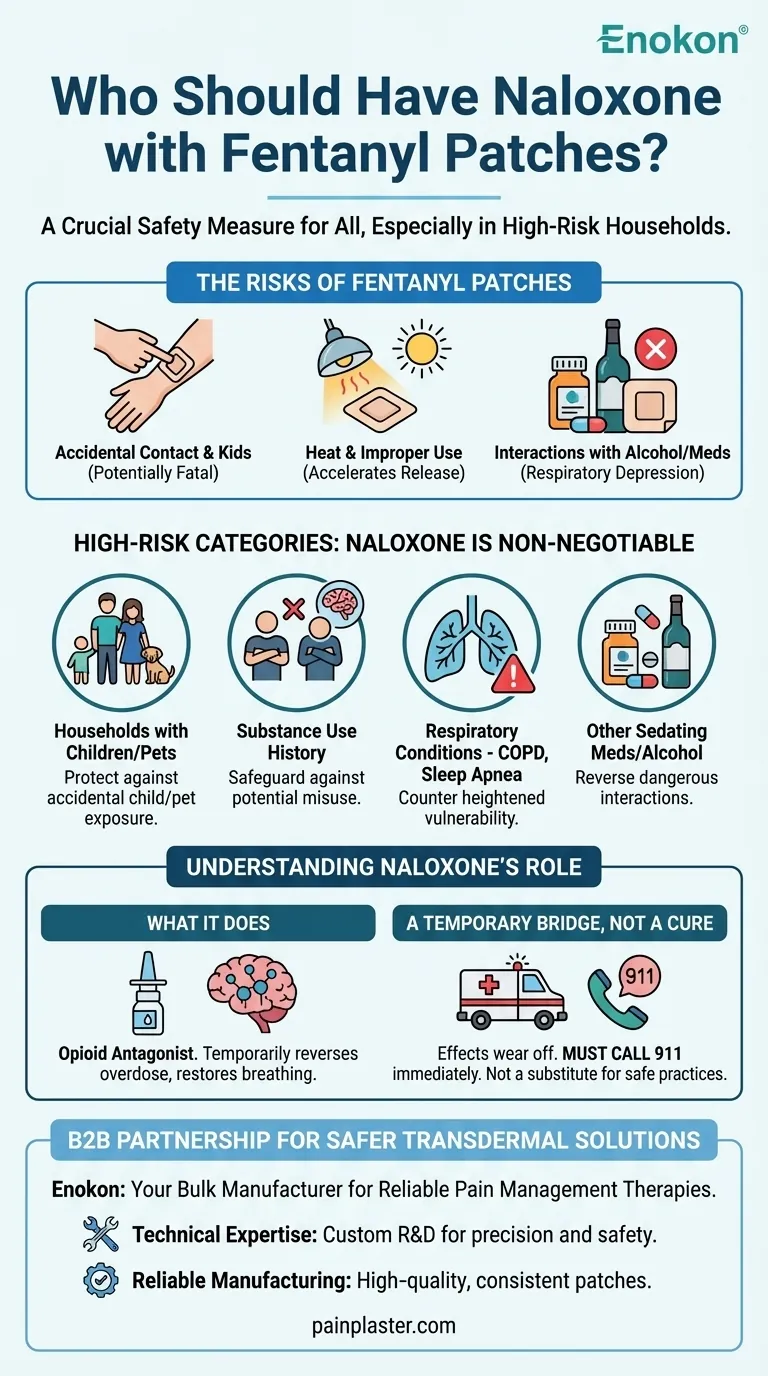
The Underlying Risks of Fentanyl Patches
Understanding why naloxone is recommended requires recognizing the specific dangers that fentanyl patches pose beyond their intended therapeutic use. These risks stem from the drug's high potency and the nature of the patch delivery system.
Risk 1: Accidental Exposure
The most common danger involves the patch unintentionally coming into contact with someone other than the patient. A loose patch can easily adhere to another person through casual contact, such as hugging.
Small children are at extreme risk. They may find a discarded or detached patch and put it in their mouth or on their skin, leading to a potentially fatal dose. Even used patches contain enough residual fentanyl to be lethal to a child.
Risk 2: Unintentional Patient Overdose
The patient themselves can experience an overdose even when trying to follow instructions. Several factors can dangerously increase the rate at which fentanyl is absorbed into the body.
Exposing the patch to a heat source—like a heating pad, electric blanket, or even a hot bath or direct sunlight—can accelerate drug release and cause an overdose. Applying more than one patch at a time without explicit medical direction is also extremely dangerous.
Risk 3: Dangerous Interactions
Fentanyl's effects, particularly respiratory depression (slowed or stopped breathing), can be dangerously amplified by other substances.
Consuming alcohol or taking other medications that cause drowsiness, such as sedatives, tranquilizers, or other opioids, can lead to a severe and unpredictable interaction. It is essential to disclose all medications, supplements, and substances you use to your doctor.
Who Is in a High-Risk Category?
While every fentanyl user should discuss naloxone with their doctor, certain situations elevate the risk profile significantly, making naloxone a non-negotiable safety tool.
Households with Children or Pets
The risk of a child finding a lost or improperly discarded patch cannot be overstated. Their small body size and lack of tolerance make any exposure a medical emergency. Keeping naloxone on hand provides a vital first-response capability.
Living with Individuals with Substance Use History
If anyone in the home has a current or past history of substance abuse, the presence of a potent opioid like fentanyl creates a high-stakes environment. Naloxone is an essential safeguard against potential misuse or diversion of the medication.
Patients with Certain Medical Conditions
Individuals with pre-existing conditions that affect breathing, such as COPD or sleep apnea, are more vulnerable to fentanyl's respiratory-depressing effects. Likewise, conditions affecting the liver or kidneys can alter how the drug is processed, increasing overdose risk.
Understanding Naloxone's Role
Having naloxone is a critical part of a comprehensive safety plan, but it's important to understand what it does and, more importantly, what it does not do.
What Naloxone Does
Naloxone is an opioid antagonist. It works by knocking opioids off the receptors in the brain, which can temporarily reverse an overdose and restore normal breathing in someone whose breathing has slowed or stopped.
It Is a Bridge, Not a Cure
The effects of naloxone are temporary and may wear off before the opioids have fully left the body. It is absolutely critical to call 911 immediately before or after administering naloxone. The person can fall back into an overdose state and will require professional medical attention.
It Does Not Replace Safe Practices
Naloxone is a last line of defense, not a substitute for responsible medication management. Meticulous attention to the safe application, storage, and disposal of fentanyl patches remains the primary way to prevent an emergency.
Making the Right Choice for Your Safety
Your decision to have naloxone should be based on a clear-eyed assessment of your specific household and health profile, made in consultation with your doctor.
- If your household includes children: You should view naloxone as an essential safety tool, similar to a fire extinguisher, to protect against accidental exposure.
- If you or someone in your home has a history of substance use: Having naloxone is a non-negotiable precaution to prevent a fatal outcome from potential misuse.
- If you have underlying health conditions or take other sedating medications: Your personal risk of overdose is elevated, making a discussion about a naloxone prescription with your doctor a critical priority.
- If you are a caregiver for a fentanyl patch user: You should be trained on recognizing the signs of an overdose and how to administer naloxone.
Equipping yourself with naloxone is a responsible and empowering step toward protecting yourself and those around you from the inherent risks of powerful opioid therapy.
Summary Table:
| High-Risk Category | Why Naloxone is Critical |
|---|---|
| Households with Children or Pets | Protects against accidental exposure from a lost or discarded patch, which can be fatal. |
| Living with Individuals with Substance Use History | Safeguards against potential misuse or diversion of the potent medication. |
| Patients with Respiratory Conditions (e.g., COPD, Sleep Apnea) | Counters heightened vulnerability to fentanyl's life-threatening respiratory depression. |
| Patients Taking Other Sedating Medications or Alcohol | Reverses dangerous, unpredictable interactions that can lead to an overdose. |
Ensure Patient Safety with Reliable Transdermal Solutions
As a bulk manufacturer of reliable transdermal patches for healthcare and pharmaceutical distributors, Enokon understands that medication safety is paramount. If you are developing or distributing pain management therapies, partner with us to benefit from:
- Technical Expertise: Our custom R&D ensures your transdermal delivery systems are developed with precision and safety in mind.
- Reliable Manufacturing: We produce high-quality, consistent fentanyl and other analgesic patches you can trust.
Let's work together to create safer medication solutions. Contact our team today to discuss your custom patch development needs.
Visual Guide
Related Products
- Far Infrared Deep Heat Relief Patches Medicated Pain Relief Patches
- Icy Hot Menthol Medicine Pain Relief Patch
- Far Infrared Heat Pain Relief Patches Transdermal Patches
- Heating Pain Relief Patches for Menstrual Cramps
- Menthol Gel Pain Relief Patch
People Also Ask
- How do pain relief patches compare to other pain relief methods? Discover Targeted, Long-Lasting Relief
- How do Deep Heat Pain Relief Patches provide pain relief? Discover the Drug-Free Mechanism
- How do pain relief patches provide targeted relief? Discover the Science Behind Effective Pain Management
- How effective are pain relief patches for muscle pain? Target Localized Pain with Transdermal Delivery
- How quickly does the Deep Heat Pain Relief Back Patch activate and how long does it provide warmth? Get 16-Hour Relief
















