Ex vivo biological membranes are utilized in diffusion experiments primarily to replicate real-world physiological environments within a controlled laboratory setting. By using tissues such as sheep nasal mucosa or skin, researchers can accurately simulate how a drug formulation interacts with and penetrates biological barriers. This process is essential for validating the specific performance advantages of microemulsions before proceeding to live clinical trials.
Core Takeaway While synthetic models exist, ex vivo biological membranes provide the necessary physiological complexity to accurately predict drug absorption. They are the standard for quantifying how the physical properties of microemulsions—specifically small particle size and low interfacial tension—translate into actual therapeutic delivery.
Simulating the Physiological Environment
Replicating Biological Barriers
To develop effective transdermal drugs, you must understand how they interact with living tissue.
Ex vivo membranes, such as sheep nasal mucosa or skin, serve as a proxy for human tissue. They retain the complex structural properties of biological barriers that synthetic filters simply cannot mimic.
Validating Microemulsion Mechanics
Microemulsions are designed with specific physical advantages, notably ultra-low interfacial tension and small particle size.
Using ex vivo membranes allows researchers to prove that these physical properties actually lead to better penetration. The biological tissue tests whether the formulation can successfully navigate cellular layers to deliver the drug.
Quantifying Penetration Performance
The Role of Franz Diffusion Cells
These experiments are typically conducted using Franz diffusion cells.
This equipment holds the biological membrane in place between a donor chamber (containing the drug) and a receptor chamber. It creates a controlled system to monitor the movement of the drug through the tissue over time.
Key Metrics: Flux and Permeability
The primary goal of these experiments is to generate hard data.
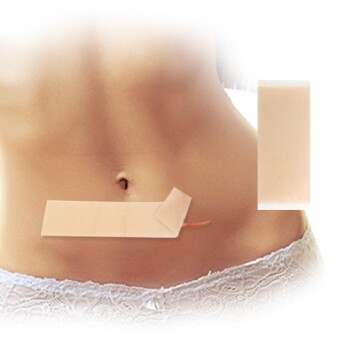
Researchers look for diffusion flux (how much drug passes through) and permeability coefficients (the rate of transport). This data supports the development of high-efficiency products like transdermal patches or sprays.
Understanding the Trade-offs and Alternatives
The Cost of Biological Accuracy
While ex vivo membranes (like sheep mucosa) offer high physiological relevance, they can be variable.
Biological tissues naturally vary from sample to sample. This variability requires rigorous experimental design to ensure data consistency, but the payoff is data that closely reflects clinical reality.
Preliminary Screening Models
For early-stage testing, utilizing full ex vivo mammalian tissue may be resource-intensive.
Acid-treated eggshell membranes offer a cost-effective alternative. They retain semi-permeable characteristics similar to mammalian skin and serve as a standardized model. While less physiologically complex than mucosal tissue, they are excellent for preliminary laboratory screening to evaluate general diffusion efficiency before moving to more advanced models.
Making the Right Choice for Your Goal
Depending on your stage of development, you should select the membrane model that aligns with your specific data requirements.
- If your primary focus is validating final formulation efficacy: Use ex vivo biological membranes (e.g., sheep skin/mucosa) to generate data on permeability coefficients and flux that reflects real physiological behavior.
- If your primary focus is preliminary high-throughput screening: Use acid-treated eggshell membranes to quickly and cost-effectively evaluate diffusion efficiency and rule out ineffective formulations early.
By matching the membrane model to your development phase, you ensure both cost-efficiency and data reliability.
Summary Table:
| Membrane Type | Primary Application | Key Benefits |
|---|---|---|
| Ex Vivo Biological | Clinical Validation | High physiological relevance; replicates real tissue barriers. |
| Eggshell (Acid-treated) | Preliminary Screening | Cost-effective; standardized model for early-stage testing. |
| Synthetic Models | Basic Quality Control | High consistency; ideal for simple diffusion rate comparisons. |
Partner with Enokon for Advanced Transdermal Solutions
As a trusted manufacturer and R&D expert, Enokon specializes in high-performance transdermal drug delivery. Whether you are developing complex microemulsions or seeking wholesale manufacturing, we provide the expertise to turn your formulations into market-ready products.
Our Capabilities Include:
- Custom R&D: Tailored solutions for specific drug penetration needs.
- Diverse Product Range: Expert production of Lidocaine, Menthol, Capsicum, Herbal, and Far Infrared pain relief patches, plus Eye Protection, Detox, and Medical Cooling Gel patches (excluding microneedle technology).
- Quality Assurance: Wholesale manufacturing that meets rigorous global standards.
Ready to elevate your product line? Contact us today to discuss your project and see how our manufacturing excellence can benefit your brand.
References
- GK Sahu, Chanchal Deep Kaur. Advancements in Microemulsion Based Drug Delivery Systems for Better Therapeutic Effects. DOI: 10.17352/ijpsdr.000003
This article is also based on technical information from Enokon Knowledge Base .
Related Products
- Menthol Gel Pain Relief Patch
- Lidocaine Hydrogel Pain Relief Patch for Pain Relief
- Asthma Cough and Pain Relief Patch for Adults and Kids
- Far Infrared Heat Pain Relief Patches Transdermal Patches
- Icy Hot Menthol Medicine Pain Relief Patch
People Also Ask
- What should be done if a dose of menthol patch is missed? Key Steps for Safe Use
- What is the primary use of a menthol patch? Targeted Relief for Muscle & Joint Pain
- How does menthol work in the Reliever Patch? Dual-Action Pain Relief Explained
- What should be avoided while using a menthol patch? Key Safety Tips for Effective Pain Relief
- What important precautions should be taken with menthol topical? Safety Guide for Effective Use