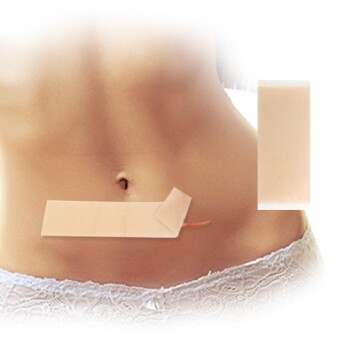
Deaeration is the fundamental process of removing entrapped air bubbles generated during the intense mixing of transdermal patch ingredients. It is a non-negotiable manufacturing step because trapped air pockets compromise the physical durability of the final film, disrupt surface uniformity, and, most critically, alter the precision of the drug delivery mechanism.
Core Takeaway The presence of microscopic air voids introduces variability in film density and thickness. This variability undermines the predictability of the drug release profile, potentially turning a precision medical device into an unreliable product.
Preserving Physical Integrity
The Consequence of Mixing
The mixing process required to blend active pharmaceutical ingredients (APIs) with polymers inevitably introduces air into the solution.
If these bubbles are not removed before the casting and drying phases, they become permanent voids within the solid structure.
Reducing Structural Weakness
The primary reference indicates that these trapped air pockets significantly reduce the structural strength of the dry film.
Voids act as stress points within the polymer matrix. Under tension—such as when a patient applies the patch—these weak points can cause the film to tear, crack, or delaminate, rendering it unusable.
Ensuring Geometric Precision
The Necessity of Even Thickness
Transdermal films rely on precise geometry to hold a specific amount of drug per square centimeter.
Air bubbles displace the actual formulation, creating inconsistent volume throughout the mixture.
Impact on Coating Uniformity
If the solution remains aerated during the coating process, the resulting dry film will have uneven thickness.
This physical irregularity makes it impossible to guarantee that a specific size of the cut film contains the exact dosage required.
Guaranteeing Clinical Performance
Stabilizing the Release Profile
The most critical function of a transdermal patch is to deliver medication at a controlled, predictable rate.
The primary reference emphasizes that trapped air negatively impacts the accuracy of this drug release profile.
The Diffusion Barrier
Air pockets interrupt the continuous polymer matrix through which the drug must diffuse.
These interruptions create unpredictable barriers or pathways, causing the drug to release either too slowly or with significant variability, which compromises clinical efficacy and patient safety.
Understanding the Processing Trade-offs
Viscosity vs. Time
While deaeration is critical, it introduces complexity regarding production time and formulation viscosity.
Thicker, more viscous formulations hold onto air bubbles more stubbornly than thin liquids.
The Cost of Rushing
Removing these bubbles requires dedicated time, often utilizing vacuum or centrifugation techniques, which extends the manufacturing cycle.
However, skipping or rushing this step to save time results in high rejection rates due to visible defects or failed dissolution testing.
Making the Right Choice for Your Goal
To ensure your transdermal product meets regulatory and functional standards, consider the following specific impacts of deaeration:
- If your primary focus is Physical Durability: Prioritize deaeration to eliminate voids that act as stress concentrators, preventing tears during application.
- If your primary focus is Dosage Accuracy: Prioritize deaeration to ensure a uniform film thickness, which guarantees that every square centimeter contains the exact intended amount of API.
- If your primary focus is Clinical Efficacy: Prioritize deaeration to maintain a consistent polymer matrix, ensuring the drug release profile matches your theoretical models.
Eliminating air is not just about aesthetics; it is the baseline requirement for a predictable and safe medical device.
Summary Table:
| Impact Category | Problem Caused by Air Voids | Consequence for Final Product |
|---|---|---|
| Physical Integrity | Stress points and structural voids | Film tearing, cracking, or delamination |
| Geometric Precision | Inconsistent formulation volume | Uneven thickness and inaccurate dosage per cm² |
| Clinical Performance | Interrupted polymer matrix | Unpredictable drug release profiles and reduced efficacy |
| Production Quality | Visible surface defects | High rejection rates and failed dissolution testing |
Elevate Your Transdermal Product Quality with Enokon
At Enokon, we understand that precision in manufacturing is the foundation of clinical success. As a trusted manufacturer and wholesale partner, we specialize in high-quality transdermal drug delivery solutions, including Lidocaine, Menthol, Capsicum, Herbal, and Far Infrared pain relief patches, as well as Eye Protection, Detox, and Medical Cooling Gel patches.
Our advanced R&D and manufacturing processes ensure rigorous deaeration and structural integrity—excluding microneedle technology—to provide your customers with reliable, safe, and effective medical-grade products. Whether you need custom R&D or wholesale supply, our team is ready to deliver excellence.
Ready to optimize your product line? Contact us today to discuss your custom transdermal solutions!
References
- Ashish Kandalkar, Subhasri Mohapatra. Effect of permeation enhancer on bioavailability of formulated patches of amoxicillin. DOI: 10.53730/ijhs.v6ns2.8417
This article is also based on technical information from Enokon Knowledge Base .
Related Products
- Menthol Gel Pain Relief Patch
- Lidocaine Hydrogel Pain Relief Patch for Pain Relief
- Asthma Cough and Pain Relief Patch for Adults and Kids
- Far Infrared Heat Pain Relief Patches Transdermal Patches
- Icy Hot Menthol Medicine Pain Relief Patch
People Also Ask
- What should be done if a dose of menthol patch is missed? Key Steps for Safe Use
- What are the serious side effects of menthol patch that require immediate medical attention?
- What should be avoided while using a menthol patch? Key Safety Tips for Effective Pain Relief
- How does menthol work in the Reliever Patch? Dual-Action Pain Relief Explained
- What important precautions should be taken with menthol topical? Safety Guide for Effective Use