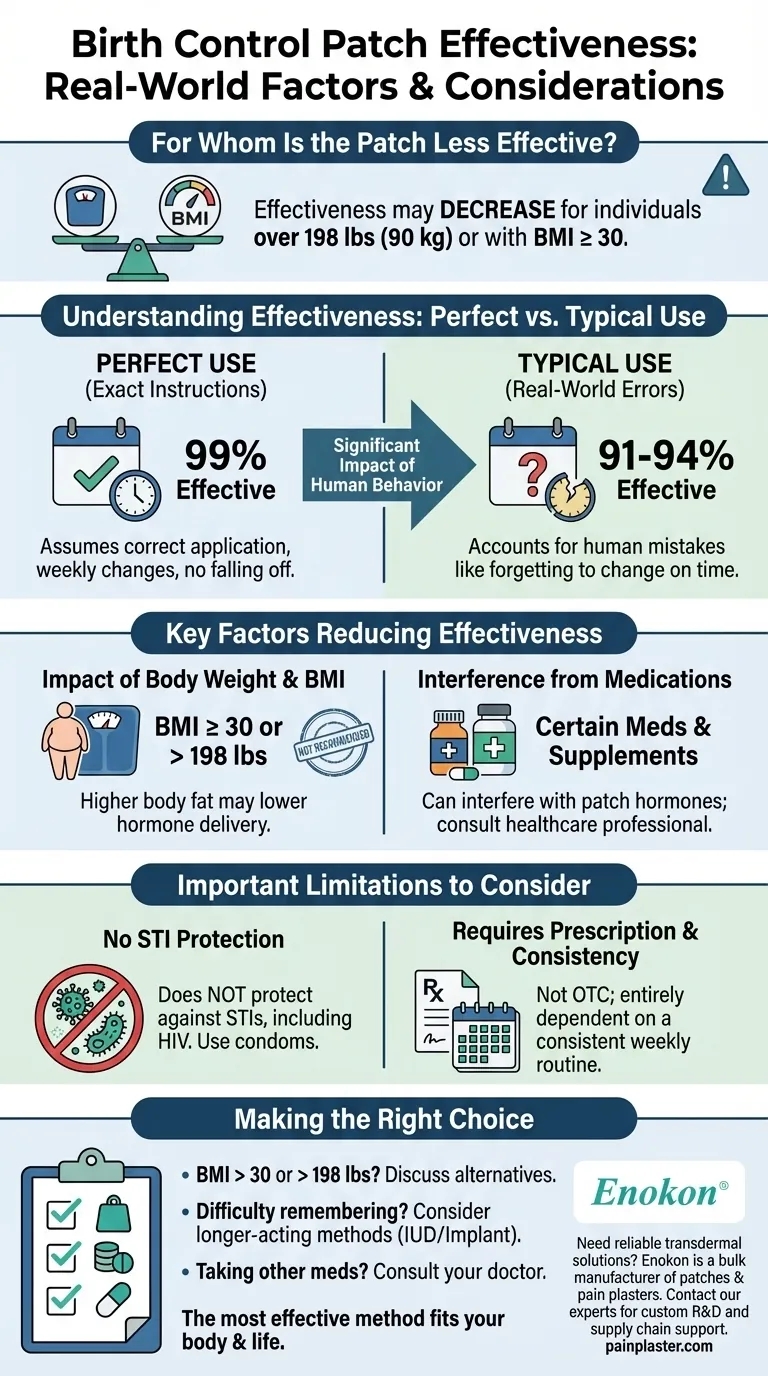
For certain individuals, the birth control patch may not provide the same level of pregnancy protection. Its effectiveness is known to decrease for women who weigh more than 198 pounds (90 kg) or have a Body Mass Index (BMI) of 30 or greater.
The reliability of the birth control patch depends on both physiological factors, like body weight, and behavioral factors, like using it exactly as directed. Understanding the difference between its "perfect use" and "typical use" effectiveness is critical for anyone considering this method.

Understanding Effectiveness: Perfect vs. Typical Use
To make an informed choice, it's essential to grasp the two ways effectiveness is measured. These numbers reveal the significant impact of real-world human behavior on contraceptive reliability.
What "Perfect Use" Means
With perfect use, which means following the instructions exactly without any mistakes, the birth control patch is 99% effective.
This high rate of effectiveness assumes the patch is applied on the correct day, changed on time every week, and never accidentally falls off.
The Reality of "Typical Use"
In the real world, mistakes happen. Typical use effectiveness accounts for human error, such as forgetting to change the patch on time.
Because of these potential mistakes, the patch's effectiveness drops to between 91% and 94%. This means that out of 100 people using the patch for a year, between 6 and 9 could become pregnant.
Key Factors That Reduce Patch Effectiveness
Beyond the difference in usage patterns, specific factors can directly lower the patch's ability to prevent pregnancy.
The Impact of Body Weight and BMI
The most clearly identified factor is body composition. The patch may deliver a lower dose of hormones in individuals with more body fat, reducing its effectiveness.
For this reason, it is not recommended for those with a BMI of 30 or more and may be less effective for anyone weighing over 198 pounds (90 kg).
Interference from Other Medications
Certain medications and supplements can interfere with the hormones in the birth control patch, making it less effective.
It is crucial to discuss all medications you are taking, including over-the-counter drugs and herbal supplements, with a healthcare professional before starting the patch.
Important Limitations to Consider
While the patch is a highly effective method for many, it has clear boundaries and requirements that must be understood.
No Protection Against STIs
The birth control patch offers no protection against sexually transmitted infections (STIs), including HIV.
Consistent and correct use of condoms is necessary to reduce the risk of STI transmission.
Requires a Prescription and Consistency
The patch is not an over-the-counter product and requires a prescription from a healthcare provider. This ensures it is a medically appropriate option for you.
Its effectiveness is also entirely dependent on a consistent weekly routine of changing the patch on the same day each week.
Making the Right Choice for Your Goal
Selecting a contraceptive method is a personal decision based on your health, lifestyle, and priorities.
- If your BMI is over 30 or you weigh more than 198 lbs: It is critical to discuss alternative, more reliable birth control options with your doctor.
- If you find it difficult to remember a weekly task: A longer-acting method that requires less frequent attention, like an IUD or implant, may be a more effective choice for you.
- If you take other medications: You must consult with your healthcare provider to ensure there are no interactions that would compromise the patch's effectiveness.
Ultimately, the most effective birth control method is one that fits your body and your life, and is used correctly and consistently.
Summary Table:
| Factor | Impact on Effectiveness | Recommendation |
|---|---|---|
| Weight > 198 lbs / BMI ≥ 30 | May be less effective; not recommended. | Consult a doctor for alternative methods. |
| Typical Use (Human Error) | Effectiveness drops to 91-94%. | Set reminders for weekly changes. |
| Certain Medications | Can interfere with hormones. | Disclose all medications to your doctor. |
Need a reliable transdermal solution for your patients or brand?
At Enokon, we are a bulk manufacturer of reliable transdermal patches and pain plasters for healthcare and pharmaceutical distributors and brands. Our technical expertise ensures high-quality, consistent hormone delivery and effective pain relief.
Benefit from our custom R&D and development services to create a product that meets specific patient needs, including considerations for dosage and efficacy across different user profiles.
Contact our experts today to discuss how we can support your product development and supply chain.
Visual Guide
Related Products
- Prostate Pain Kidney Health Care Patch for Men
- Menthol Gel Pain Relief Patch
- Capsaicin Chili Medicated Pain Relief Patches
- Lidocaine Hydrogel Pain Relief Patch for Pain Relief
- Far Infrared Deep Heat Relief Patches Medicated Pain Relief Patches
People Also Ask
- What precautions should be taken when applying testosterone patches? Maximize Safety and Effectiveness
- What should be done before undergoing an MRI while using testosterone patches? Remove it to prevent serious burns.
- What should be done in case of a testosterone patch overdose? A Step-by-Step Emergency Guide
- How often should testosterone patches be applied? Daily Dosage & Best Practices
- What is the purpose of testosterone patches? A Steady Solution for Low Testosterone















