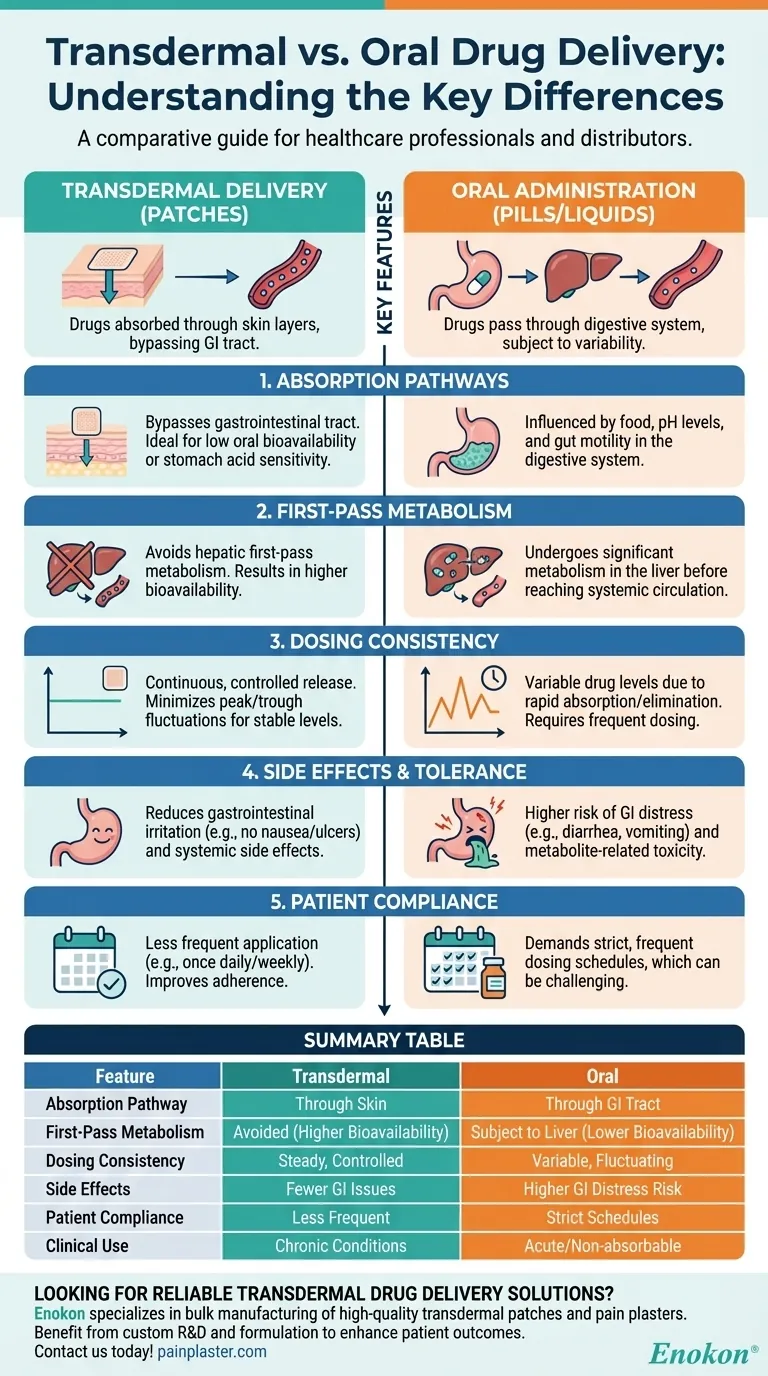
Transdermal drug delivery and oral administration are two distinct methods of delivering medications, each with unique mechanisms, advantages, and limitations. Transdermal delivery involves administering drugs through the skin, typically via patches, while oral administration delivers drugs through the gastrointestinal tract. The key differences lie in absorption pathways, metabolic effects, dosing consistency, and patient compliance. Transdermal methods avoid first-pass metabolism, provide steady drug levels, and reduce gastrointestinal side effects, whereas oral administration is simpler but subject to digestive variability and hepatic metabolism.

Key Points Explained:
-
Absorption Pathways
- Transdermal: Drugs are absorbed through the skin layers into systemic circulation, bypassing the gastrointestinal tract. This method is ideal for drugs with low oral bioavailability or those degraded by stomach acid.
- Oral: Drugs pass through the digestive system, where absorption is influenced by factors like food intake, pH levels, and gut motility.
-
First-Pass Metabolism
- Transdermal: Avoids hepatic first-pass metabolism, leading to higher bioavailability (e.g., transdermal oxybutynin has 80% bioavailability vs. lower rates for oral forms).
- Oral: Undergoes first-pass metabolism in the liver, which can significantly reduce the active drug concentration before it reaches systemic circulation.
-
Dosing Consistency
- Transdermal: Provides continuous, controlled release (e.g., transdermal drug patch), minimizing peak/trough fluctuations (e.g., rivastigmine patch maintains stable plasma levels).
- Oral: Often results in variable drug levels due to rapid absorption and elimination, requiring frequent dosing.
-
Side Effects and Tolerance
- Transdermal: Reduces gastrointestinal irritation (e.g., no nausea or ulcers) and systemic side effects (e.g., lower DEO metabolite levels for oxybutynin).
- Oral: More likely to cause GI distress (e.g., diarrhea, vomiting) and higher metabolite-related toxicity.
-
Patient Compliance
- Transdermal: Patches require less frequent application (e.g., once daily or weekly), improving adherence.
- Oral: Demands strict scheduling (e.g., multiple daily doses), which can be challenging for patients.
-
Clinical Applications
- Transdermal: Preferred for chronic conditions (e.g., pain management, hormone therapy) where steady drug levels are critical.
- Oral: Suitable for acute treatments or drugs that cannot be formulated for skin absorption.
-
Dose Conversion
- Transdermal patches often require specific dose adjustments when switching from oral forms (e.g., rivastigmine patch doses are tailored to prior oral intake).
By understanding these differences, healthcare providers and purchasers can select the optimal delivery method based on drug properties, patient needs, and therapeutic goals. Transdermal systems, though often costlier, offer advantages for long-term therapies where consistency and tolerability are paramount.
Summary Table:
| Feature | Transdermal Delivery | Oral Administration |
|---|---|---|
| Absorption Pathway | Through skin layers into systemic circulation | Through gastrointestinal tract |
| First-Pass Metabolism | Avoids hepatic metabolism (higher bioavailability) | Subject to liver metabolism (lower bioavailability) |
| Dosing Consistency | Steady, controlled release (e.g., patches) | Variable absorption (peak/trough fluctuations) |
| Side Effects | Fewer GI issues (e.g., no nausea) | Higher risk of GI distress (e.g., ulcers) |
| Patient Compliance | Less frequent application (e.g., weekly patches) | Requires strict dosing schedules |
| Clinical Use | Chronic conditions (pain, hormones) | Acute treatments or non-absorbable drugs |
Looking for reliable transdermal drug delivery solutions? Enokon specializes in bulk manufacturing of high-quality transdermal patches and pain plasters for healthcare distributors and brands. Benefit from our expertise in custom R&D and formulation to enhance patient outcomes. Contact us today to discuss your project needs!
Visual Guide
Related Products
- Natural Herbal Wormwood Patch Pain Plaster
- Icy Hot Menthol Medicine Pain Relief Patch
- Capsaicin Chili Medicated Pain Relief Patches
- Mugwort Wormwood Pain Relief Patch for Neck Pain
- Heating Pain Relief Patches for Menstrual Cramps
People Also Ask
- What precautions should be taken when using pain relief patches? Essential Safety Guide
- How do pain relief patches provide targeted relief? Discover the Science Behind Effective Pain Management
- Can pregnant women use pain relief patches? Your Essential Guide to Safe Pain Management
- When should the pain relief patch not be used? Key Safety Rules to Avoid Risks
- What medical conditions should be reported before using buprenorphine patches? Essential Safety Guide