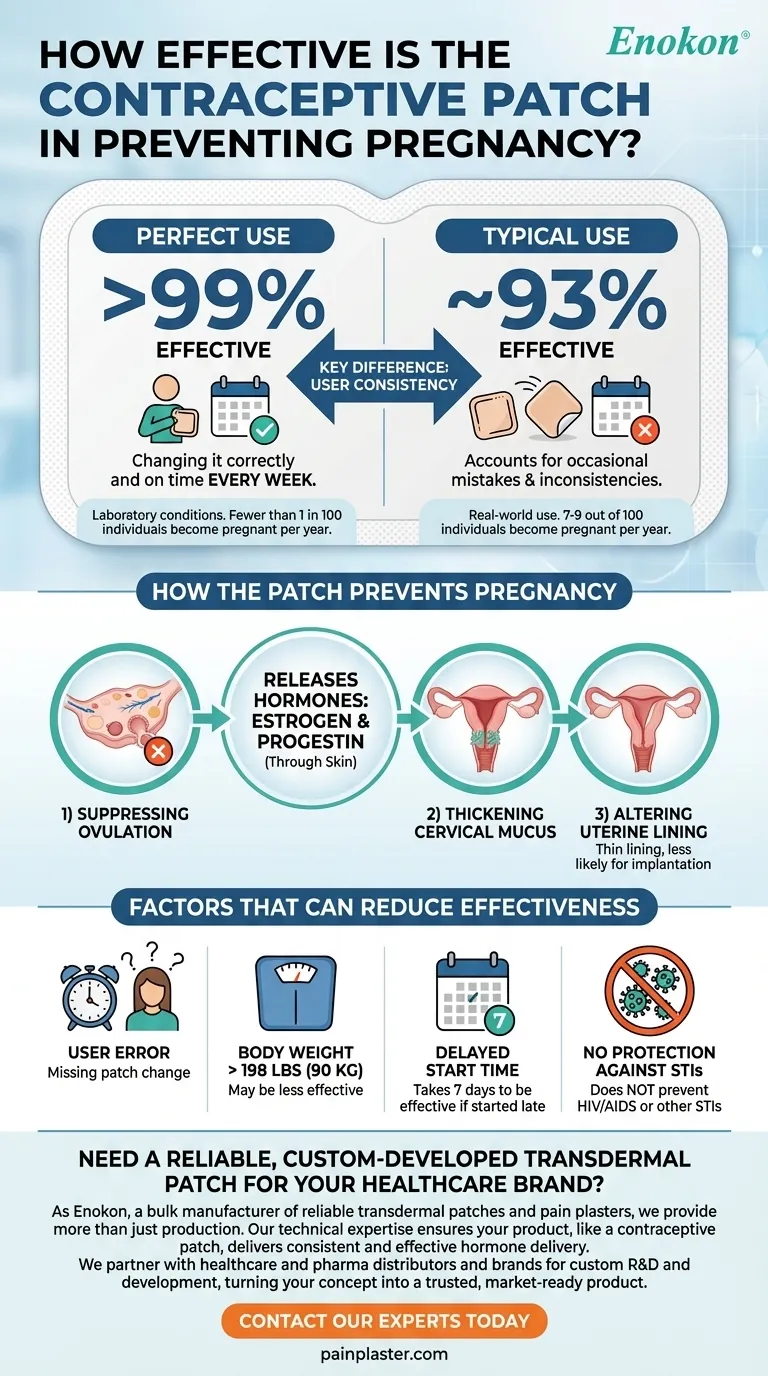
The contraceptive patch is a highly effective method of birth control, but its real-world success rate depends entirely on how consistently it is used. With perfect use—changing it correctly and on time every week—the patch is over 99% effective at preventing pregnancy. However, with typical, real-world use that accounts for occasional mistakes, its effectiveness drops to about 93%.
The key difference between the patch being 99% effective versus 93% effective comes down to one factor: user consistency. The technology is reliable, but its success hinges on your ability to remember to change the patch on time.

How the Patch Prevents Pregnancy
The birth control patch works by releasing a steady dose of two hormones, estrogen and progestin, directly through your skin. These are the same hormones found in many combination birth control pills.
Suppressing Ovulation
The primary way the patch prevents pregnancy is by stopping your ovaries from releasing an egg each month (a process called ovulation). If no egg is released, fertilization cannot occur.
Thickening Cervical Mucus
The hormones also cause the mucus around your cervix to thicken. This creates a natural barrier that makes it significantly more difficult for sperm to enter the uterus and reach any potential egg.
Altering the Uterine Lining
Finally, the hormones can thin the lining of the uterus. This makes it less likely that a fertilized egg could attach and develop, providing an additional layer of protection.
"Perfect Use" vs. "Typical Use": What the Numbers Mean
The difference between over 99% and 93% effectiveness is crucial for anyone relying on the patch for contraception. This gap is not about the patch failing, but about human error.
The Ideal Scenario: Perfect Use (>99% Effective)
Perfect use means using the patch exactly as directed without any mistakes. This involves changing your patch on the same designated day each week and applying a new one on time after your patch-free week.
Under these laboratory-perfect conditions, fewer than 1 in 100 individuals will become pregnant in a year.
The Reality: Typical Use (93% Effective)
Typical use reflects how people use birth control in the real world. It accounts for common mistakes like forgetting to change the patch on time or the patch accidentally coming loose.
With typical use, about 7 to 9 out of 100 individuals will experience an unintended pregnancy in a year. This drop in effectiveness is almost entirely due to inconsistent application.
Factors That Can Reduce Effectiveness
While highly reliable when used correctly, certain factors can compromise the patch's ability to prevent pregnancy. Understanding these is critical for success.
User Error
The single biggest reason for failure is not applying a new patch on time. A delay of even a day or two can reduce its effectiveness.
Body Weight
The patch may be less effective for individuals who weigh more than 198 pounds (90 kg). The dosage of hormones absorbed may not be sufficient to reliably prevent ovulation in those with a higher body mass.
Delayed Start Time
When you first start using the patch, it is not immediately effective. It takes seven full days for the hormones to build up to a protective level in your body unless you start it within the first five days of your menstrual period.
No Protection Against STIs
It is essential to remember that the contraceptive patch offers zero protection against HIV (AIDS) or any other sexually transmitted infections (STIs).
Making the Right Choice for Your Situation
To decide if the patch is the right method for you, consider how its requirements align with your lifestyle and health profile.
- If your primary focus is maximum reliability: You must be committed to changing the patch on the exact same day each week to achieve its >99% effectiveness rate.
- If you struggle with weekly routines: Be aware that the patch's real-world effectiveness can drop to 93%, and you may want to discuss lower-maintenance options with your doctor.
- If you weigh more than 198 pounds (90kg): You must consult a healthcare provider to discuss whether the patch is a suitable and effective option for you.
Understanding these factors empowers you to use the patch correctly or choose the birth control method that best fits your life.
Summary Table:
| Effectiveness Scenario | Success Rate | Key Factor |
|---|---|---|
| Perfect Use | >99% | Changing the patch correctly and on time every week. |
| Typical Use | ~93% | Accounts for common user errors, like forgetting to change it. |
| Primary Mechanism | Stops ovulation, thickens cervical mucus, and thins uterine lining. | Releases estrogen and progestin through the skin. |
Need a reliable, custom-developed transdermal patch for your healthcare brand?
As Enokon, a bulk manufacturer of reliable transdermal patches and pain plasters, we provide more than just production. Our technical expertise ensures your product, like a contraceptive patch, delivers consistent and effective hormone delivery. We partner with healthcare and pharma distributors and brands for custom R&D and development, turning your concept into a trusted, market-ready product.
Let's discuss your project requirements. Contact our experts today to explore how we can support your brand's success.
Visual Guide
Related Products
- Prostate Pain Kidney Health Care Patch for Men
- Capsaicin Chili Medicated Pain Relief Patches
- Far Infrared Deep Heat Relief Patches Medicated Pain Relief Patches
- Lidocaine Hydrogel Pain Relief Patch for Pain Relief
- Icy Hot Menthol Medicine Pain Relief Patch
People Also Ask
- What precautions should be taken when applying testosterone patches? Maximize Safety and Effectiveness
- What should be done in case of a testosterone patch overdose? A Step-by-Step Emergency Guide
- What should be done before undergoing an MRI while using testosterone patches? Remove it to prevent serious burns.
- What should be done if a testosterone patch falls off? A Guide to Maintaining Hormone Stability
- What should patients tell their doctor before using testosterone patches? A Guide to Safe Treatment















