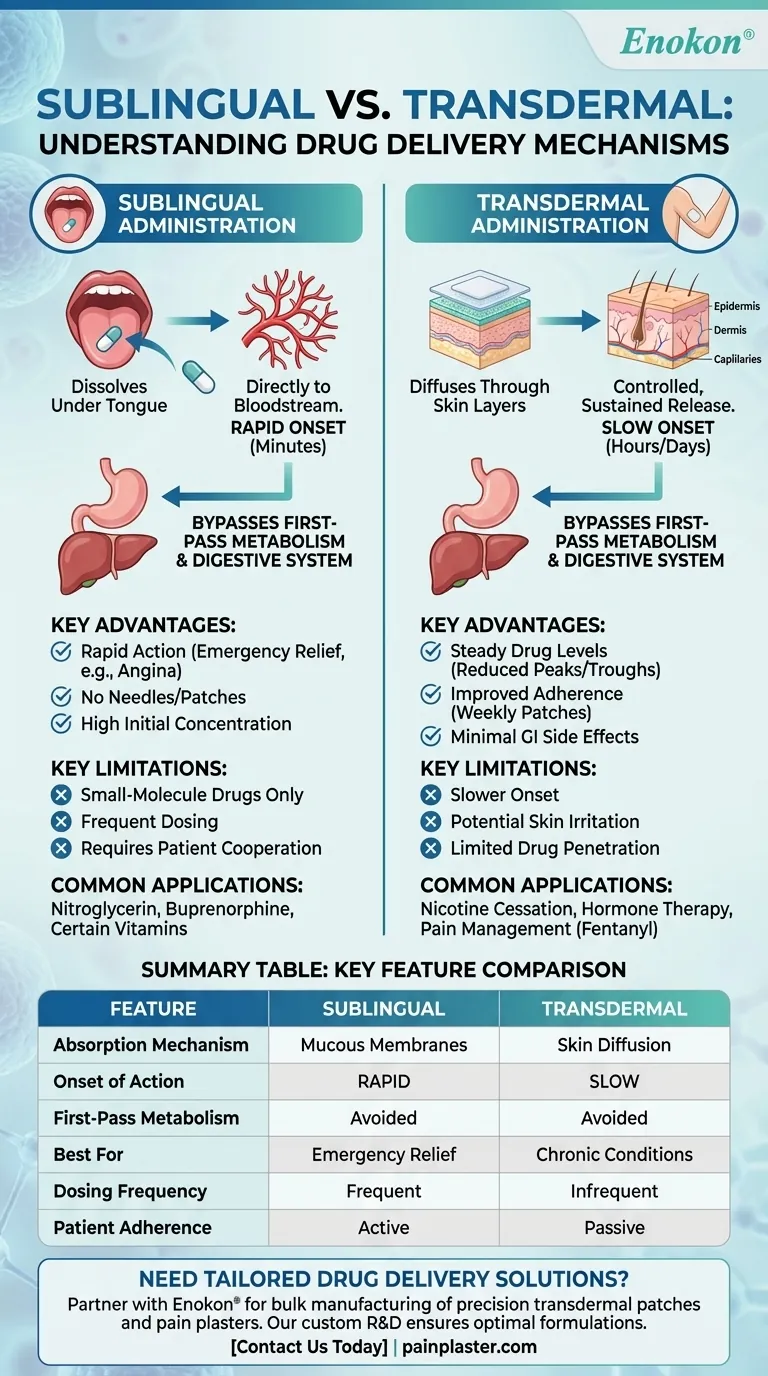
Sublingual and transdermal drug administration are two distinct methods with unique mechanisms, advantages, and clinical applications. Sublingual administration involves placing a drug under the tongue, where it dissolves and is absorbed directly into the bloodstream via the rich vascular network of the mucous membranes. This method bypasses the gastrointestinal tract and first-pass metabolism, offering rapid onset of action. Transdermal administration, on the other hand, delivers drugs through the skin via patches, providing controlled, sustained release over time. It also avoids first-pass metabolism but involves slower absorption through the epidermis. Each method is suited for specific drug types and clinical scenarios, with sublingual being ideal for quick relief and transdermal for long-term, steady dosing.
Key Points Explained:
-
Mechanism of Absorption
- Sublingual: Drugs dissolve in saliva and are absorbed through the mucous membranes under the tongue, entering the bloodstream directly. This bypasses the digestive system and liver metabolism, ensuring faster onset (often within minutes).
- Transdermal: Drugs diffuse through the skin’s outer layers (epidermis and dermis) into capillaries. Absorption is slower but sustained, as patches release medication over hours or days (e.g., 24-hour patches like the 4.6 mg or 9.5 mg doses mentioned).
-
Advantages and Limitations
-
Sublingual:
- Pros: Rapid action (critical for emergencies like angina or allergic reactions), avoids stomach acid degradation, and simplifies administration (no needles or patches).
- Cons: Limited to small-molecule drugs that can dissolve quickly; not suitable for long-term dosing.
-
Transdermal:
- Pros: Steady drug levels (reducing peaks/troughs), minimal gastrointestinal side effects, and improved compliance (e.g., weekly patches).
- Cons: Slower onset, potential skin irritation, and limited to drugs that can penetrate the skin effectively.
-
Sublingual:
-
Clinical Applications
- Sublingual: Used for nitroglycerin (angina), buprenorphine (pain), and certain vitamins/hormones. Ideal when immediate effects are needed.
- Transdermal: Common for nicotine cessation, hormone therapy (estrogen), and pain management (fentanyl patches). Suited for chronic conditions requiring consistent dosing.
-
Patient-Specific Considerations
- Switching from oral to transdermal (as in the reference example) requires careful dose conversion to maintain efficacy. For instance, a 6–12 mg oral dose may translate to a 9.5 mg/24-hour patch.
- Sublingual routes demand patient cooperation (holding the drug under the tongue), while transdermal patches offer passive adherence but require proper skin application.
-
Pharmacokinetic Differences
- Sublingual drugs achieve higher initial concentrations but shorter duration.
- Transdermal systems maintain therapeutic levels longer, reducing dosing frequency.
These methods exemplify how drug delivery innovations cater to diverse therapeutic needs—whether for urgent relief or sustained management—showcasing the quiet yet transformative role of pharmaceutical technologies in healthcare.
Summary Table:
| Feature | Sublingual Administration | Transdermal Administration |
|---|---|---|
| Absorption Mechanism | Dissolves in saliva, absorbed via mucous membranes | Diffuses through skin layers into capillaries |
| Onset of Action | Rapid (minutes) | Slow (hours to days) |
| First-Pass Metabolism | Avoided | Avoided |
| Best For | Emergency relief (e.g., angina) | Chronic conditions (e.g., pain, hormone therapy) |
| Dosing Frequency | Frequent (short duration) | Infrequent (sustained release) |
| Patient Adherence | Requires active cooperation | Passive (patch application) |
Need tailored drug delivery solutions? Partner with Enokon, a trusted bulk manufacturer of precision transdermal patches and pain plasters for healthcare brands and distributors. Our expertise in custom R&D ensures optimal formulations for your clinical needs—whether rapid sublingual action or controlled transdermal release. Contact us today to discuss your project!
Visual Guide
Related Products
- Far Infrared Heat Pain Relief Patches Transdermal Patches
- Heating Pain Relief Patches for Menstrual Cramps
- Capsaicin Chili Medicated Pain Relief Patches
- Icy Hot Menthol Medicine Pain Relief Patch
- Menthol Gel Pain Relief Patch
People Also Ask
- How quickly does the Deep Heat Pain Relief Back Patch activate and how long does it provide warmth? Get 16-Hour Relief
- What did the UK Million Women Study find regarding transdermal versus oral hormone therapy? A Safer Choice for Gallbladder Health
- Can heat patches be used for fresh injuries? Avoid This Common Mistake for Faster Recovery
- What are the key features of the Deep Heat Pain Relief Back Patch? Get Up to 16 Hours of Drug-Free Relief
- What types of pain can the Deep Heat Pain Relief Back Patch be used for? Targeted Relief for Muscles & Joints













