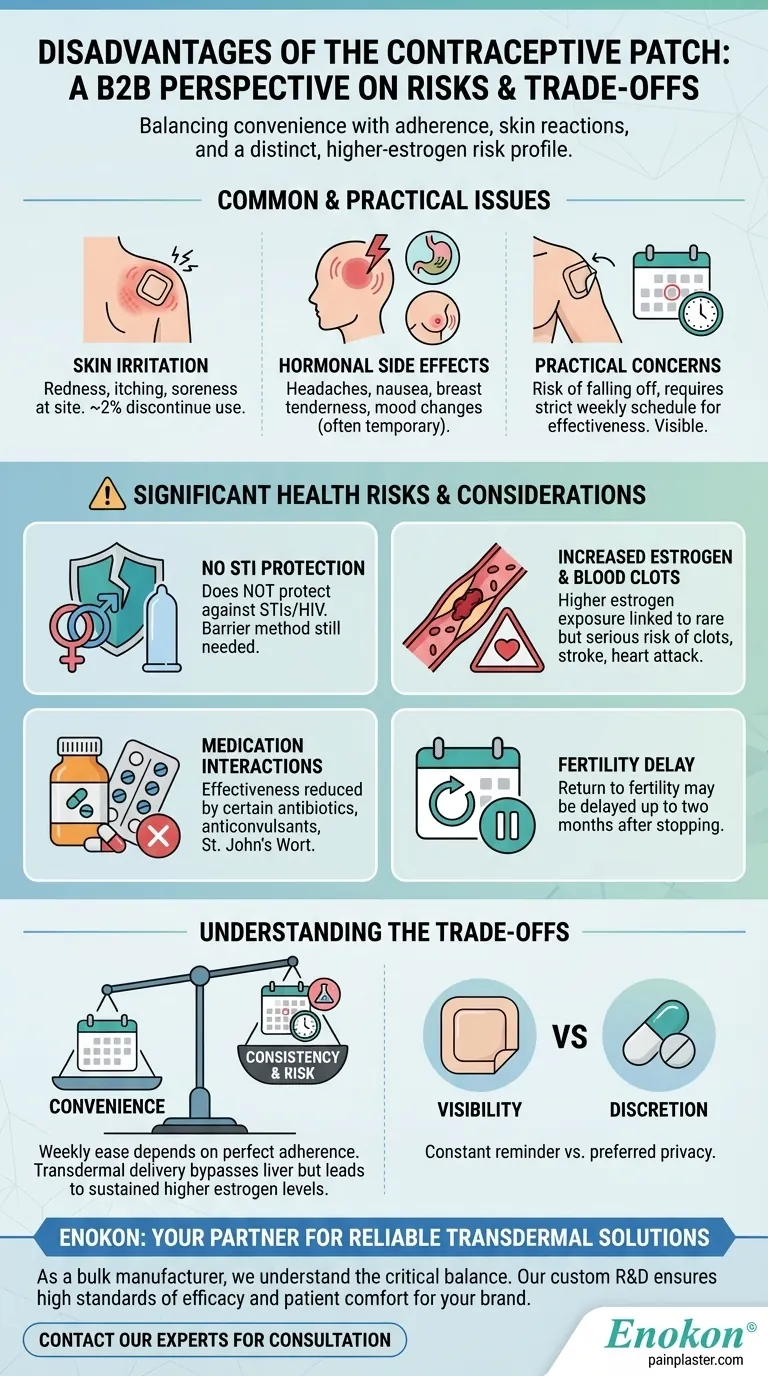
While convenient, the contraceptive patch has notable disadvantages including skin irritation, common hormonal side effects like nausea and headaches, and practical issues like the risk of it falling off. More significantly, it offers no protection against STIs, exposes users to higher estrogen levels than some other methods, and carries a rare but serious risk of blood clots.
The core trade-off of the contraceptive patch is its weekly convenience versus the need for perfect adherence and a distinct risk profile, driven by higher estrogen exposure compared to many combination pills.

The Most Common Disadvantages
The most frequently reported issues are manageable but can impact your daily life and comfort. Understanding these upfront is key to deciding if the patch is a sustainable option for you.
Skin Irritation at the Application Site
Many users experience some form of skin reaction where the patch is applied. This can range from mild itching and redness to soreness.
For a small number of women, about 2 out of 100, this irritation is significant enough to cause them to discontinue using the patch.
Hormonal Side Effects
Like many hormonal contraceptives, the patch can cause side effects, especially during the first few months as your body adjusts.
These commonly include breast tenderness, headaches, nausea, mood changes, and spotting or bleeding between periods. While often temporary, they can be disruptive.
Practical and Lifestyle Concerns
The patch is a visible form of birth control, which may be a concern for some users, and it can sometimes be felt by a partner.
There is also the risk of the patch becoming loose or falling off, which compromises its effectiveness. It requires a consistent weekly schedule; forgetting to change it on time reduces its ability to prevent pregnancy.
Significant Health Risks and Considerations
Beyond the common side effects, the patch carries several important health considerations that require a conversation with your healthcare provider.
No Protection Against STIs
This is a critical limitation. The contraceptive patch does not protect against sexually transmitted infections (STIs), including HIV.
If STI protection is a concern, you must use a barrier method like a condom in addition to the patch.
Increased Estrogen Exposure
The patch delivers a higher overall dose of estrogen into the bloodstream compared to many combination birth control pills.
This higher level of estrogen is directly linked to some of the more serious health risks associated with the patch.
Risk of Serious Complications
While rare, the patch increases the risk of serious and potentially life-threatening blood clots. These can lead to a pulmonary embolism (a clot in the lung), heart attack, or stroke.
Long-term use may also be associated with a slightly increased risk of developing breast cancer and cervical cancer.
Interactions with Other Medications
The patch's effectiveness can be reduced by certain medications and supplements.
Key interactions include the antibiotic rifampin, anticonvulsants, corticosteroids, and the herbal supplement St. John's Wort.
Potential Delay in Fertility
After you stop using the patch, your return to normal fertility may be delayed. It can take up to two months for your regular cycle to resume.
Understanding the Trade-offs
Choosing a contraceptive method is about balancing effectiveness, convenience, and risk. The patch presents a unique set of these trade-offs.
Convenience vs. Consistency
The "set it and forget it" nature of a weekly patch is appealing compared to a daily pill.
However, this convenience is entirely dependent on perfect consistency. Forgetting the single weekly change has a greater impact on effectiveness than forgetting one daily pill.
Transdermal Delivery vs. Systemic Risk
Delivering hormones through the skin allows them to bypass initial processing by the liver, but it also results in higher, more sustained estrogen levels in the body.
This is the primary reason for the elevated risk of blood clots compared to some other hormonal methods.
Visibility vs. Discretion
The patch is a constant, visible reminder of your contraception choice.
This lack of discretion is a significant downside for some, who may prefer an oral pill, an injection, or a long-acting internal device like an IUD.
Making the Right Choice for Your Goal
Your personal health profile and lifestyle priorities will determine if the patch's disadvantages outweigh its benefits.
- If your primary focus is avoiding a daily pill: The patch is a viable alternative, but only if you can commit to a strict weekly schedule and have no contraindications.
- If you have a history of blood clots, migraines with aura, or are a smoker over 35: The patch's higher estrogen dose makes it a high-risk and generally unsuitable choice.
- If your priority is maximum discretion or you have sensitive skin: The patch's visibility and potential for skin irritation may make other methods more appealing.
- If you require robust STI protection: You must supplement the patch with condoms or another barrier method every time you have sex.
Ultimately, an informed conversation with your healthcare provider is the essential next step to safely match a birth control method to your specific needs.
Summary Table:
| Disadvantage | Key Details |
|---|---|
| Skin Irritation | Redness, itching, soreness at application site; 2% of users discontinue use. |
| Hormonal Side Effects | Headaches, nausea, breast tenderness, mood changes (often temporary). |
| Serious Health Risks | Increased risk of blood clots, heart attack, stroke due to higher estrogen exposure. |
| No STI Protection | Does not protect against sexually transmitted infections; condoms are still needed. |
| Practical Issues | Can fall off, requires strict weekly schedule, is visible on the skin. |
| Medication Interactions | Effectiveness reduced by certain antibiotics, anticonvulsants, and St. John's Wort. |
Ready to explore reliable, custom-developed transdermal solutions?
As Enokon, a bulk manufacturer of reliable transdermal patches and pain plasters for healthcare and pharma distributors and brands, we understand the critical balance between user convenience and safety. Our technical expertise in custom R&D and development ensures that your products meet the highest standards of efficacy and patient comfort.
Let's discuss how we can support your brand with innovative, high-quality transdermal delivery systems. Contact our experts today for a consultation.
Visual Guide
Related Products
- Prostate Pain Kidney Health Care Patch for Men
- Capsaicin Chili Medicated Pain Relief Patches
- Far Infrared Deep Heat Relief Patches Medicated Pain Relief Patches
- Lidocaine Hydrogel Pain Relief Patch for Pain Relief
- Icy Hot Menthol Medicine Pain Relief Patch
People Also Ask
- What lifestyle factors should be considered when choosing between testosterone patches and injections? Find Your Best Fit
- How often should testosterone patches be applied? Daily Dosage & Best Practices
- What should be done if a dose of testosterone patches is missed? Regain Stability and Safety
- What should be done if a testosterone patch is missed or falls off? Follow these simple timing rules for safety and consistency.
- What should be done before undergoing an MRI while using testosterone patches? Remove it to prevent serious burns.