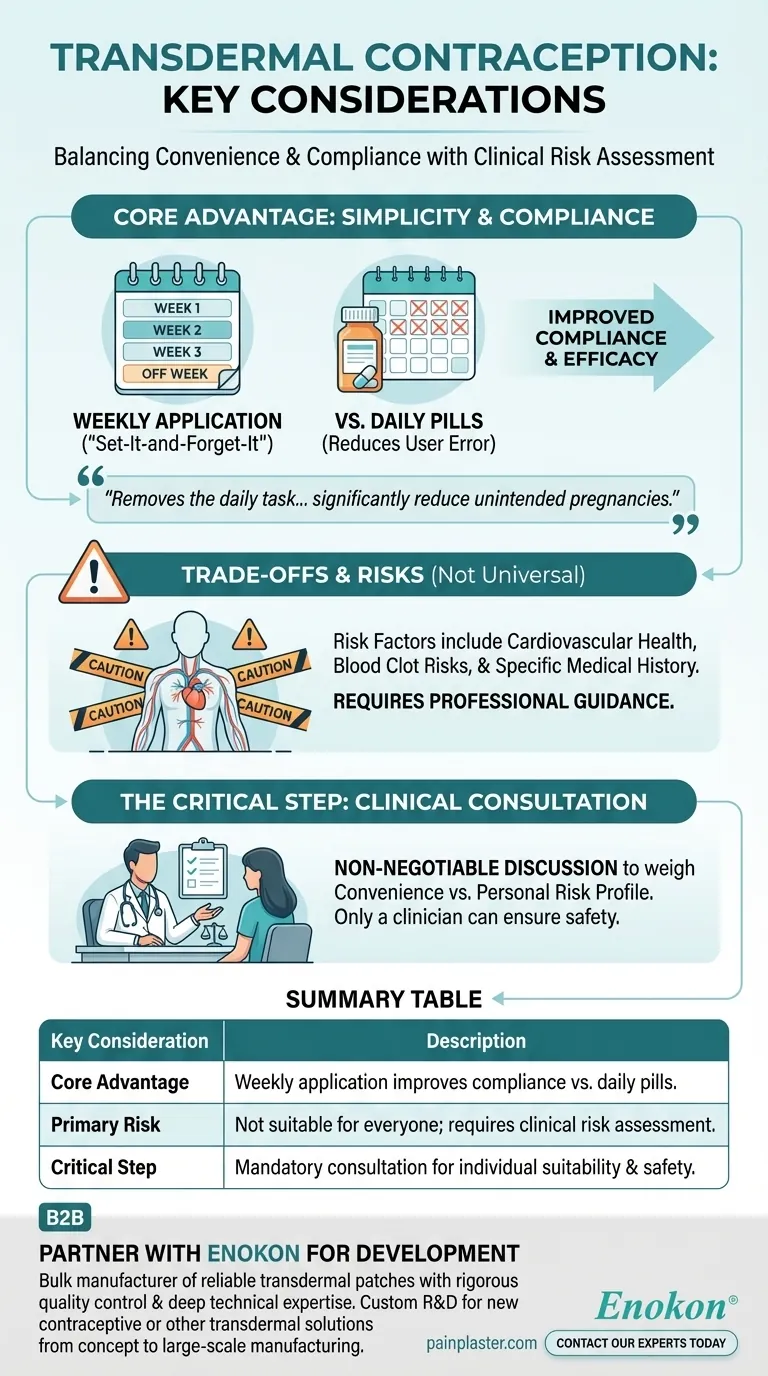
The primary considerations for transdermal contraception are its significant convenience and potential for improved compliance compared to daily methods, balanced against the critical need for a clinical risk assessment. The patch is an important option for many, but it is not universally suitable and requires a thorough discussion with a healthcare provider to ensure it is a safe choice for your specific health profile.
The contraceptive patch excels by removing the daily task of taking a pill, which can significantly reduce unintended pregnancies caused by human error. However, this convenience must be weighed against individual health risks that only a clinician can properly evaluate.

The Core Advantage: Simplicity and Compliance
Transdermal contraception, commonly known as "the patch," offers a distinct operational model compared to more traditional methods like the oral pill. Its main value proposition is ease of use.
A "Set-It-and-Forget-It" Method
The patch is typically applied once a week for three consecutive weeks, followed by a patch-free week. This weekly schedule eliminates the need for a daily reminder.
This simple routine is a powerful feature for individuals who find it difficult to adhere to a strict daily medication schedule.
The Compliance Factor
The single most common reason for contraceptive failure among pill users is forgetting to take it. By reducing the frequency of action from daily to weekly, the patch minimizes the opportunity for such errors.
This improved compliance is directly linked to higher efficacy in real-world use, potentially leading to fewer unintended pregnancies.
A Viable Alternative
For those who have struggled with the daily demands of oral contraceptives, the patch provides an important and effective alternative. It offers the same hormonal regulation without the same memory burden.
Understanding the Trade-offs and Risks
While the patch is a powerful tool, it is not a one-size-fits-all solution. Its hormonal delivery mechanism comes with specific contraindications that must be taken seriously.
Not a Universal Solution
The patch is not suitable for everyone. Certain pre-existing health conditions or lifestyle factors can make its use unsafe.
This is why transdermal contraception is a prescription method that requires professional medical guidance.
The Importance of Risk Factors
Women with certain risk factors cannot use the patch. These conditions are typically related to cardiovascular health, blood clot risks, and other specific medical histories.
A clinician will conduct a thorough review of your personal and family medical history to identify any potential dangers.
The Non-Negotiable Clinical Consultation
An open discussion with your doctor is the most critical step. This conversation is designed to weigh the benefits of the patch's convenience against your personal risk profile.
Only a qualified healthcare provider can help you make a truly informed decision about whether this method is appropriate and safe for you.
How to Apply This to Your Goal
Your final decision should be guided by a clear understanding of your personal priorities and health status, made in partnership with your healthcare provider.
- If your primary focus is convenience and you struggle with daily medication: The patch offers a major advantage by improving compliance, which is a key factor in contraceptive effectiveness.
- If you have any pre-existing health conditions or a complex medical history: A thorough consultation with your clinician is absolutely essential to determine if you are a suitable candidate for the patch.
- If you are simply exploring new contraceptive options: View the patch as a strong contender that simplifies your routine, but be prepared to engage in a detailed risk-benefit analysis with your doctor.
Ultimately, understanding both the convenience and the necessary precautions empowers you to have the most productive conversation possible with your healthcare provider.
Summary Table:
| Key Consideration | Description |
|---|---|
| Core Advantage | Weekly application improves compliance vs. daily pills, reducing user error and unintended pregnancies. |
| Primary Risk | Not suitable for everyone; requires a clinical risk assessment for conditions like cardiovascular or blood clot issues. |
| Critical Step | A non-negotiable consultation with a healthcare provider is mandatory to determine individual suitability and safety. |
Partner with Enokon for Your Transdermal Product Development
As a bulk manufacturer of reliable transdermal patches for leading healthcare and pharma distributors and brands, Enokon combines rigorous quality control with deep technical expertise. Whether you are developing a new contraceptive patch or another innovative transdermal solution, our custom R&D and development services ensure a product that is both effective and safe for end-users.
Contact our experts today to discuss how we can support your project from concept to compliant, large-scale manufacturing.
Visual Guide
Related Products
- Far Infrared Heat Pain Relief Patches Transdermal Patches
- Capsaicin Chili Medicated Pain Relief Patches
- Herbal Eye Protection Patch Eye Patch
- Heating Pain Relief Patches for Menstrual Cramps
- Menthol Gel Pain Relief Patch
People Also Ask
- How do Deep Heat Pain Relief Patches provide pain relief? Discover the Drug-Free Mechanism
- How does capsaicin work in the medicated heat patch? The Science Behind Pain Relief
- What types of pain can the Deep Heat Pain Relief Back Patch be used for? Targeted Relief for Muscles & Joints
- Can heat patches be used for fresh injuries? Avoid This Common Mistake for Faster Recovery
- What did the UK Million Women Study find regarding transdermal versus oral hormone therapy? A Safer Choice for Gallbladder Health