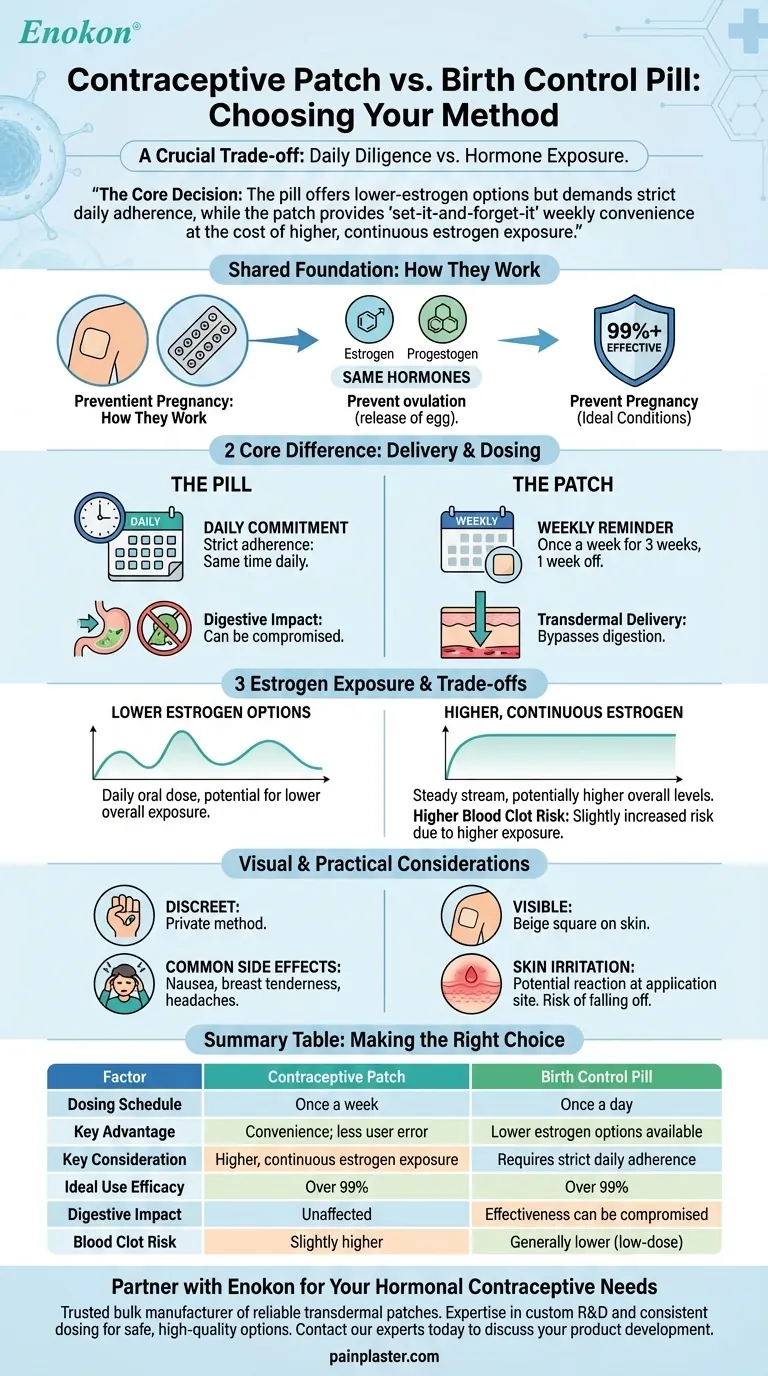
Choosing between the contraceptive patch and the pill hinges on a crucial trade-off between daily diligence and hormone exposure. Both methods are highly effective at preventing pregnancy, using the same types of hormones to do so. The primary differences lie in how frequently you use them, how the hormones enter your body, and your personal health profile.
The core decision is this: The pill offers lower-estrogen options but demands strict daily adherence, while the patch provides "set-it-and-forget-it" weekly convenience at the cost of higher, continuous estrogen exposure.

How They Work: A Shared Foundation
Both the patch and the combination pill are hormonal contraceptives that work in the same fundamental way. They are designed to prevent pregnancy with a very high degree of reliability when used correctly.
The Same Hormones, Different Paths
Both methods use two types of hormones: estrogen and progestogen. These hormones work together primarily by preventing your ovaries from releasing an egg (ovulation).
They are chemically similar, but the delivery method is the key distinction. The pill is taken orally and absorbed through your digestive system, while the patch is applied to the skin and delivers hormones transdermally.
Identical Efficacy Under Ideal Conditions
When used perfectly, both the patch and the pill are over 99% effective at preventing pregnancy. Their effectiveness is considered equal, so your choice should not be based on one being inherently better at its primary job.
The Core Difference: Delivery and Dosing
The practical experience of using the patch versus the pill is where the choice becomes clear. Your lifestyle and personal preferences will heavily influence which method is a better fit.
Daily Task vs. Weekly Reminder
The most significant difference is the schedule. The pill requires a daily commitment at the same time each day to maintain its effectiveness.
The patch is applied only once a week for three consecutive weeks, followed by a patch-free week. This significantly reduces the chance of user error for those who find a daily routine difficult to maintain.
The Impact of Digestion
Because the pill is absorbed through the stomach, its effectiveness can be compromised by vomiting or severe diarrhea.
The patch completely bypasses the digestive system. This makes it a more reliable option if you have gastrointestinal conditions that might interfere with oral medication absorption.
Estrogen Exposure: A Critical Distinction
While both contain estrogen, the patch delivers it differently. It releases a continuous, steady stream of hormones directly into the bloodstream.
Studies show this can result in your body being exposed to higher overall levels of estrogen compared to many common birth control pills. This is a critical factor for considering potential risks.
Understanding the Trade-offs
Neither method is perfect, and each comes with a distinct set of considerations. Being aware of the potential downsides is essential for making an informed choice.
The Blood Clot Risk Factor
All hormonal contraceptives containing estrogen carry a small, but serious, risk of blood clots.
Due to the higher estrogen exposure, the contraceptive patch may carry a slightly higher risk of blood clots compared to some lower-dose combined oral contraceptive pills. This is a crucial point to discuss with your doctor, especially if you have other risk factors.
Common Side Effects
Both methods can cause similar side effects common to hormonal birth control, such as breast tenderness, headaches, or nausea.
The patch has a unique potential side effect of skin irritation or a reaction at the application site.
Visual Presence and Adhesion
The pill is a discreet, private method. The patch, however, is a visible beige square on your skin.
There is also a small risk that the patch could become loose or fall off, which would require you to reapply it or apply a new one to remain protected.
Making the Right Choice for Your Lifestyle
Ultimately, the best contraceptive is the one you will use correctly and consistently. Your personal priorities should guide your conversation with your healthcare provider.
- If your primary focus is convenience and you struggle with daily routines: The weekly patch removes the daily burden and is likely a better fit for your lifestyle.
- If your primary focus is minimizing estrogen exposure or you have risk factors for blood clots: A low-dose birth control pill is generally considered the more cautious choice.
- If you have sensitive skin or want a more discreet method: The pill avoids the potential for skin irritation and is not visible to others.
- If you have digestive issues that could interfere with medication: The patch provides more reliable protection by bypassing the stomach entirely.
Discuss your health history and lifestyle honestly with your doctor to select the method that offers you the most effective and comfortable protection.
Summary Table:
| Factor | Contraceptive Patch | Birth Control Pill |
|---|---|---|
| Dosing Schedule | Once a week | Once a day |
| Key Advantage | Convenience; less user error | Lower estrogen options available |
| Key Consideration | Higher, continuous estrogen exposure | Requires strict daily adherence |
| Ideal Use Efficacy | Over 99% | Over 99% |
| Digestive Impact | Unaffected by vomiting/diarrhea | Effectiveness can be compromised |
| Blood Clot Risk | Slightly higher due to estrogen exposure | Generally lower with low-dose options |
Partner with Enokon for Your Hormonal Contraceptive Needs
As a trusted bulk manufacturer of reliable transdermal patches, Enokon understands the precise delivery and consistent dosing required for effective hormonal contraceptives. Our technical expertise in custom R&D and development ensures that healthcare and pharma brands can offer patients safe, high-quality options.
If you are a distributor or brand looking to develop or source contraceptive patches, contact our experts today to discuss how we can support your product development with our reliable manufacturing and formulation knowledge.
Visual Guide
Related Products
- Prostate Pain Kidney Health Care Patch for Men
- Capsaicin Chili Medicated Pain Relief Patches
- Far Infrared Deep Heat Relief Patches Medicated Pain Relief Patches
- Lidocaine Hydrogel Pain Relief Patch for Pain Relief
- Asthma Cough and Pain Relief Patch for Adults and Kids
People Also Ask
- How often should testosterone patches be applied? Daily Dosage & Best Practices
- What should be done if a testosterone patch falls off? A Guide to Maintaining Hormone Stability
- What should be done in case of a testosterone patch overdose? A Step-by-Step Emergency Guide
- What should patients tell their doctor before using testosterone patches? A Guide to Safe Treatment
- What should be done if a testosterone patch is missed or falls off? Follow these simple timing rules for safety and consistency.















