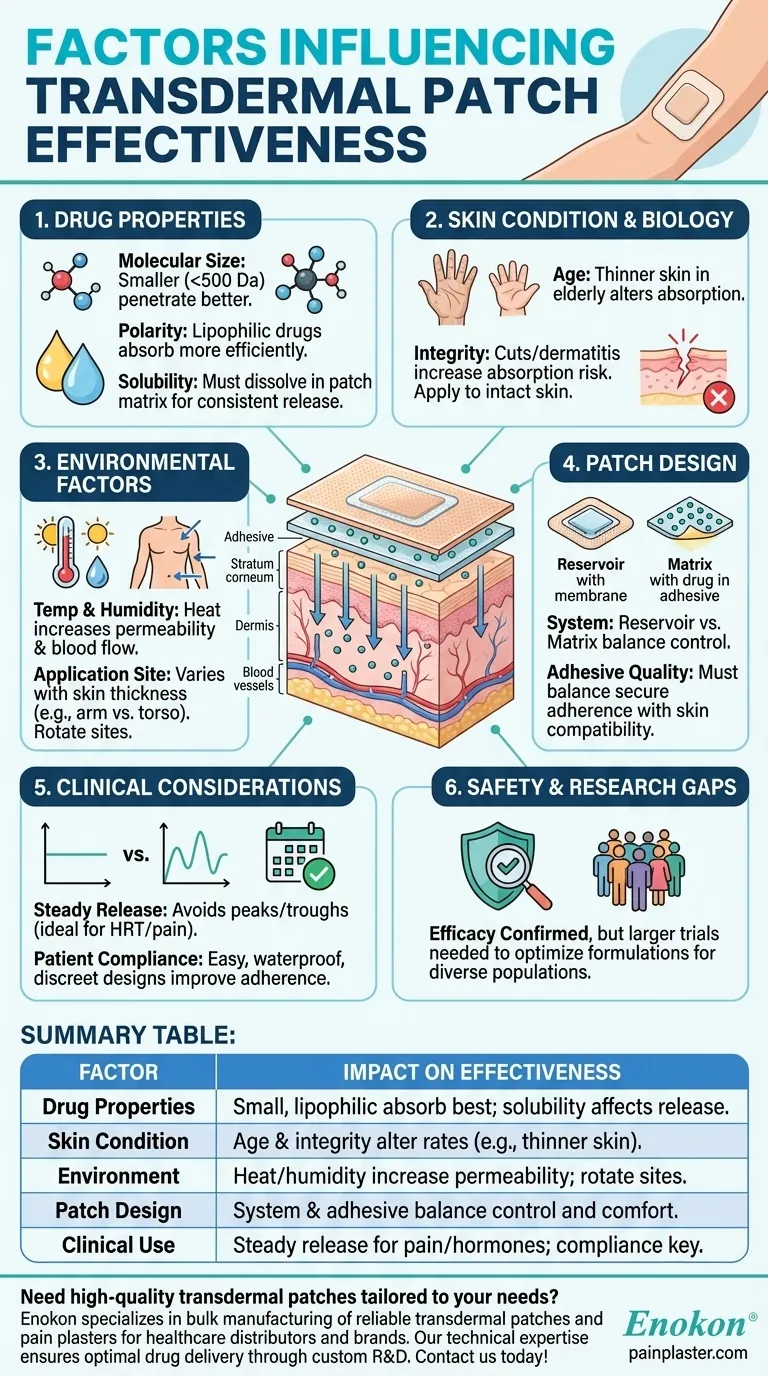
Transdermal patches are a sophisticated drug delivery system that relies on multiple factors to ensure effective medication absorption through the skin. Their effectiveness hinges on drug properties (like molecular size and polarity), skin condition, environmental factors, and patch design. These variables must be carefully balanced to achieve consistent drug release, patient comfort, and therapeutic efficacy. From hormone replacement therapy to pain management, transdermal patches offer a non-invasive, steady-release alternative to oral or injectable medications, but their success depends on meticulous formulation and application considerations.

Key Points Explained:
-
Drug Properties
- Molecular Size: Smaller molecules (typically <500 Daltons) penetrate the skin more efficiently. Larger molecules may require enhancers or alternative delivery methods.
- Polarity: Lipophilic (fat-soluble) drugs absorb better due to the skin’s lipid-rich outer layer. Hydrophilic drugs may need chemical permeation enhancers.
- Solubility: Drugs must dissolve adequately in the patch matrix for consistent release. For example, hormone replacement therapies like estrogen or testosterone (/topic/transdermal-patch) are formulated to balance solubility and skin permeability.
-
Skin Condition and Biology
- Age: Older skin is thinner and less hydrated, potentially altering absorption rates. Pediatric or geriatric patients may require adjusted dosages.
- Skin Integrity: Cuts, eczema, or dermatitis can increase absorption unpredictably, risking overdose. Patches should be applied to intact, clean skin.
-
Environmental Factors
- Temperature and Humidity: Heat increases blood flow and skin permeability, potentially accelerating drug release. High humidity can affect patch adhesion.
- Application Site: Areas with varying skin thickness (e.g., arm vs. torso) influence absorption. Rotating sites prevents skin irritation.
-
Patch Design
- Reservoir vs. Matrix Systems: Reservoir patches control release via a membrane, while matrix patches embed the drug in the adhesive. The latter simplifies design and reduces size.
- Adhesive Quality: Must balance adherence with skin compatibility. Poor adhesion risks inconsistent dosing, while harsh adhesives cause irritation.
-
Clinical Considerations
- Steady Release: Ideal for hormones (e.g., HRT) or pain management, avoiding peaks/troughs seen with oral meds.
- Patient Compliance: Easy application improves adherence, but patches must be waterproof and discreet for daily wear.
-
Safety and Research Gaps
- While studies confirm efficacy (e.g., analgesia patches), larger trials are needed to optimize formulations for diverse populations and drugs.
By addressing these factors, manufacturers can tailor transdermal patches to specific therapeutic needs, ensuring reliable delivery and patient comfort. For purchasers, evaluating these variables helps select patches that align with clinical goals and user requirements.
Summary Table:
| Factor | Impact on Effectiveness |
|---|---|
| Drug Properties | Small, lipophilic molecules absorb best; solubility affects release consistency. |
| Skin Condition | Age, hydration, and integrity alter absorption rates (e.g., thinner skin in elderly). |
| Environment | Heat/humidity increase permeability; application site rotation prevents irritation. |
| Patch Design | Matrix vs. reservoir systems balance control and comfort; adhesives must be skin-friendly. |
| Clinical Use | Steady release ideal for pain/hormones; waterproof designs improve compliance. |
Need high-quality transdermal patches tailored to your needs?
Enokon specializes in bulk manufacturing of reliable transdermal patches and pain plasters for healthcare distributors and brands. Our technical expertise ensures optimal drug delivery through custom R&D, balancing adhesion, release rates, and patient comfort. Contact us today to discuss your project requirements or request samples!
Visual Guide
Related Products
- Far Infrared Heat Pain Relief Patches Transdermal Patches
- Heating Pain Relief Patches for Menstrual Cramps
- Capsaicin Chili Medicated Pain Relief Patches
- Medical Cooling Gel Patches for Fever Cooling Patches
- Far Infrared Deep Heat Relief Patches Medicated Pain Relief Patches
People Also Ask
- How do Deep Heat Pain Relief Patches provide pain relief? Discover the Drug-Free Mechanism
- What did the UK Million Women Study find regarding transdermal versus oral hormone therapy? A Safer Choice for Gallbladder Health
- What types of pain can the Deep Heat Pain Relief Back Patch be used for? Targeted Relief for Muscles & Joints
- What are the common side effects of using the medicated heat patch? Understanding Risks & Safe Use
- Can heat patches be used for fresh injuries? Avoid This Common Mistake for Faster Recovery












