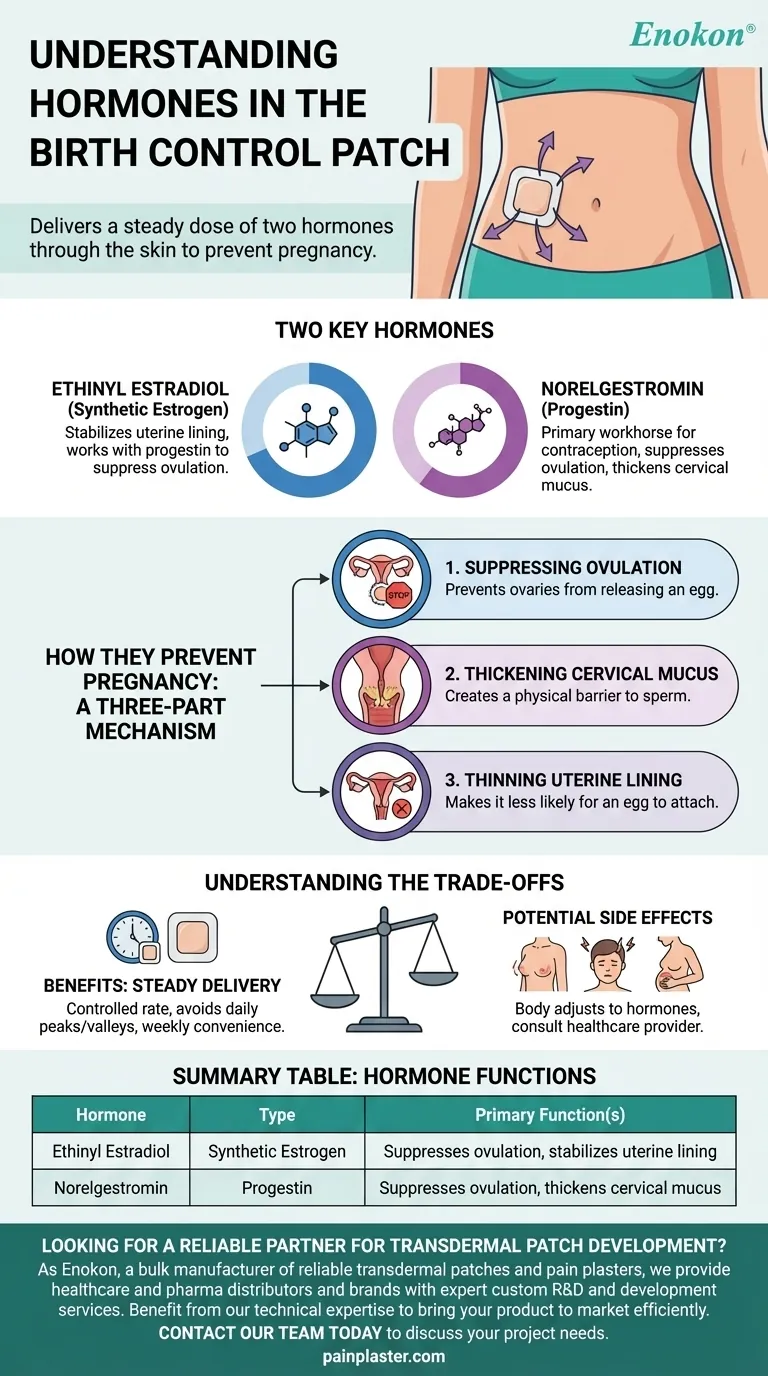
The birth control patch contains two specific hormones that work together to prevent pregnancy. These are a type of estrogen called ethinyl estradiol and a type of progestin called norelgestromin.
The patch delivers a steady dose of a specific estrogen and progestin through the skin. Understanding the distinct roles these two hormones play is the key to understanding how the patch effectively prevents pregnancy.

How These Hormones Prevent Pregnancy
The combination of estrogen and progestin in the patch prevents pregnancy through a three-part mechanism. It is designed to interrupt the normal hormonal cycle that leads to conception.
Suppressing Ovulation
The primary function of these hormones is to prevent your ovaries from releasing an egg, a process known as ovulation.
By providing a consistent level of estrogen and progestin, the patch signals to your brain that there are enough hormones in circulation. This suppresses the natural hormonal surge that would normally trigger the release of an egg each month.
Thickening Cervical Mucus
The progestin in the patch, norelgestromin, causes the mucus around the cervix to thicken.
This thicker mucus creates a physical barrier, making it significantly more difficult for sperm to travel through the cervix and reach an egg, should one be released.
Thinning the Uterine Lining
Finally, the hormones cause the lining of the uterus (the endometrium) to become thinner than it normally would during a menstrual cycle.
A thinner lining makes it less likely that a fertilized egg could attach and develop, adding another layer of protection.
Understanding the Hormones Themselves
While they work as a team, ethinyl estradiol and norelgestromin each have primary responsibilities.
Ethinyl Estradiol (The Estrogen)
Ethinyl estradiol is a synthetic form of estrogen. Its main role in the patch is to stabilize the uterine lining, which helps prevent irregular bleeding or spotting between periods.
It also works with the progestin to help suppress ovulation.
Norelgestromin (The Progestin)
Norelgestromin is the primary "workhorse" hormone for contraception in the patch.
This progestin is most responsible for preventing ovulation and thickening the cervical mucus, which are the two most powerful contraceptive effects.
Understanding the Trade-offs
Using hormonal contraception involves balancing effectiveness and convenience with how your body responds to the hormones.
The Benefit of Steady Delivery
Delivering hormones through the skin (transdermally) allows them to enter the bloodstream directly at a controlled, steady rate.
This avoids the daily hormonal peaks and valleys that can occur with a pill and only requires a weekly change, which many find more convenient.
Potential Side Effects
The hormones in the patch are also responsible for its potential side effects. These are similar to other combination hormonal methods and can include breast tenderness, headaches, or nausea as your body adjusts.
The Importance of Consultation
Because these hormones directly affect your body's endocrine system, it is essential to discuss your personal and family medical history with a healthcare provider. They can help determine if the patch is a suitable and safe option for you.
Making an Informed Decision
Choosing a birth control method is a personal decision based on your health, lifestyle, and goals.
- If your primary focus is effectiveness: The combination of ethinyl estradiol and norelgestromin makes the patch a highly effective method when used correctly.
- If your primary focus is convenience: The weekly application, enabled by the transdermal delivery of these hormones, is a significant advantage over daily methods.
- If your primary focus is managing side effects: Understanding that these two hormones drive both the benefits and potential side effects is the first step in tracking your body's response.
Knowing precisely how these hormones function empowers you to have a more productive conversation with your doctor about what is right for you.
Summary Table:
| Hormone | Type | Primary Function(s) |
|---|---|---|
| Ethinyl Estradiol | Synthetic Estrogen | Suppresses ovulation, stabilizes uterine lining |
| Norelgestromin | Progestin | Suppresses ovulation, thickens cervical mucus |
Looking for a reliable partner for transdermal patch development? As Enokon, a bulk manufacturer of reliable transdermal patches and pain plasters, we provide healthcare and pharma distributors and brands with expert custom R&D and development services. Benefit from our technical expertise to bring your product to market efficiently. Contact our team today to discuss your project needs.
Visual Guide
Related Products
- Prostate Pain Kidney Health Care Patch for Men
- Menthol Gel Pain Relief Patch
- Capsaicin Chili Medicated Pain Relief Patches
- Lidocaine Hydrogel Pain Relief Patch for Pain Relief
- Far Infrared Deep Heat Relief Patches Medicated Pain Relief Patches
People Also Ask
- What should be done before undergoing an MRI while using testosterone patches? Remove it to prevent serious burns.
- What should be done if a testosterone patch is missed or falls off? Follow these simple timing rules for safety and consistency.
- What should patients tell their doctor before using testosterone patches? A Guide to Safe Treatment
- What is the purpose of testosterone patches? A Steady Solution for Low Testosterone
- What precautions should be taken when applying testosterone patches? Maximize Safety and Effectiveness















