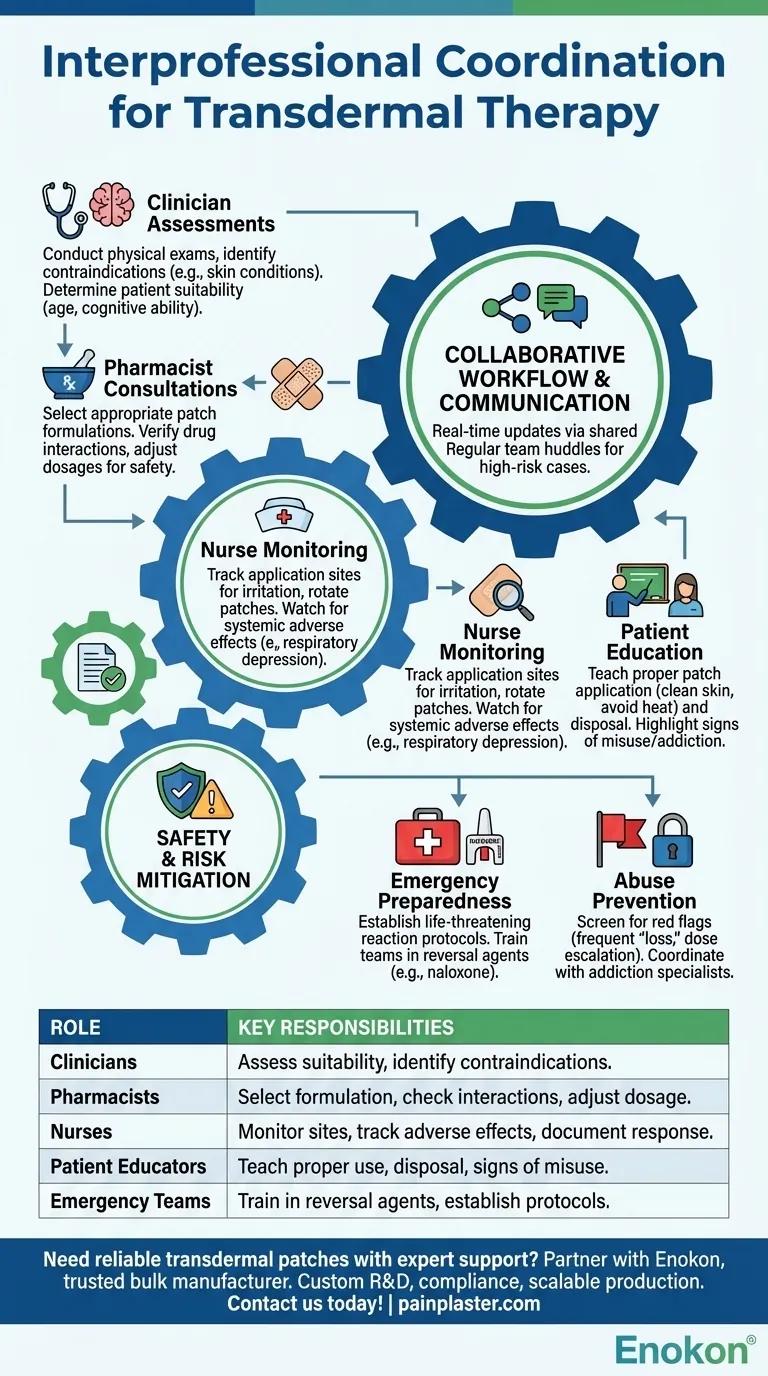
Transdermal therapy requires seamless interprofessional coordination to ensure patient safety, efficacy, and proper administration. Key roles include clinicians for initial assessments, pharmacists for drug selection, nurses for monitoring, and patient educators for adherence. Emergency protocols and misuse screening are critical, especially for opioid-based transdermal patches. Teams must be trained in reversal agents and clear communication to address adverse reactions or dependency risks.

Key Points Explained:
-
Clinician Assessments
- Conduct physical exams and update medical histories to identify contraindications (e.g., skin conditions, allergies).
- Determine if the patient is a candidate for transdermal delivery, considering factors like age, mobility, and cognitive ability.
-
Pharmacist Consultations
- Select appropriate transdermal patch formulations based on drug pharmacokinetics and patient needs (e.g., fentanyl vs. nicotine patches).
- Verify interactions with other medications and adjust dosages to prevent toxicity.
-
Nurse Monitoring
- Track application sites for irritation or absorption issues. Rotate patches to avoid skin damage.
- Watch for systemic adverse effects (e.g., respiratory depression with opioids) and document responses.
-
Emergency Preparedness
- Establish protocols for life-threatening reactions (e.g., naloxone availability for opioid overdoses).
- Train all team members in reversal agents and rapid response steps.
-
Patient Education
- Teach proper patch application (clean, dry skin; avoid heat exposure) and disposal to prevent misuse.
- Highlight signs of misuse/addiction, especially for high-risk medications.
-
Interprofessional Communication
- Use shared records for real-time updates on patient status or therapy adjustments.
- Regular team huddles to discuss high-risk cases or protocol changes.
-
Abuse Prevention
- Screen for red flags (e.g., frequent patch "loss" or dose escalation requests).
- Coordinate with addiction specialists if dependence is suspected.
This collaborative framework ensures transdermal therapy balances efficacy with safety, addressing both clinical and behavioral risks. Have you considered how workflow integration (e.g., EHR alerts) could further streamline this process? Such systems are among the quiet innovations elevating modern care.
Summary Table:
| Role | Key Responsibilities |
|---|---|
| Clinicians | Assess patient suitability, identify contraindications (e.g., skin conditions, allergies). |
| Pharmacists | Select appropriate patch formulations, check drug interactions, adjust dosages. |
| Nurses | Monitor application sites, track adverse effects, document patient responses. |
| Patient Educators | Teach proper patch use, disposal, and signs of misuse/addiction. |
| Emergency Teams | Train in reversal agents (e.g., naloxone), establish rapid response protocols. |
Need reliable transdermal patches with expert support? Partner with Enokon, a trusted bulk manufacturer of high-quality transdermal patches and pain plasters for healthcare distributors and brands. Our technical expertise ensures custom R&D, compliance, and scalable production. Contact us today to discuss your needs!
Visual Guide
Related Products
- Far Infrared Heat Pain Relief Patches Transdermal Patches
- Herbal Eye Protection Patch Eye Patch
- Heating Pain Relief Patches for Menstrual Cramps
- Menthol Gel Pain Relief Patch
- Icy Hot Menthol Medicine Pain Relief Patch
People Also Ask
- How quickly does the Deep Heat Pain Relief Back Patch activate and how long does it provide warmth? Get 16-Hour Relief
- How does the Deep Heat Back Patch work? A Drug-Free Solution for Targeted Pain Relief
- What are the common side effects of using the medicated heat patch? Understanding Risks & Safe Use
- Are heat patches safe for all body parts? Key Safety Zones and No-Go Areas Explained
- How do Deep Heat Pain Relief Patches provide pain relief? Discover the Drug-Free Mechanism















