For children in contact with an individual using topical testosterone, you must monitor for any signs of premature puberty. This unintended exposure, known as virilization, occurs through skin-to-skin contact with the medication before it has fully dried.
The central issue is the accidental transfer of a powerful hormone to a child's system. Your primary goal is not just to monitor for symptoms but to rigorously prevent any chance of exposure from occurring in the first place.

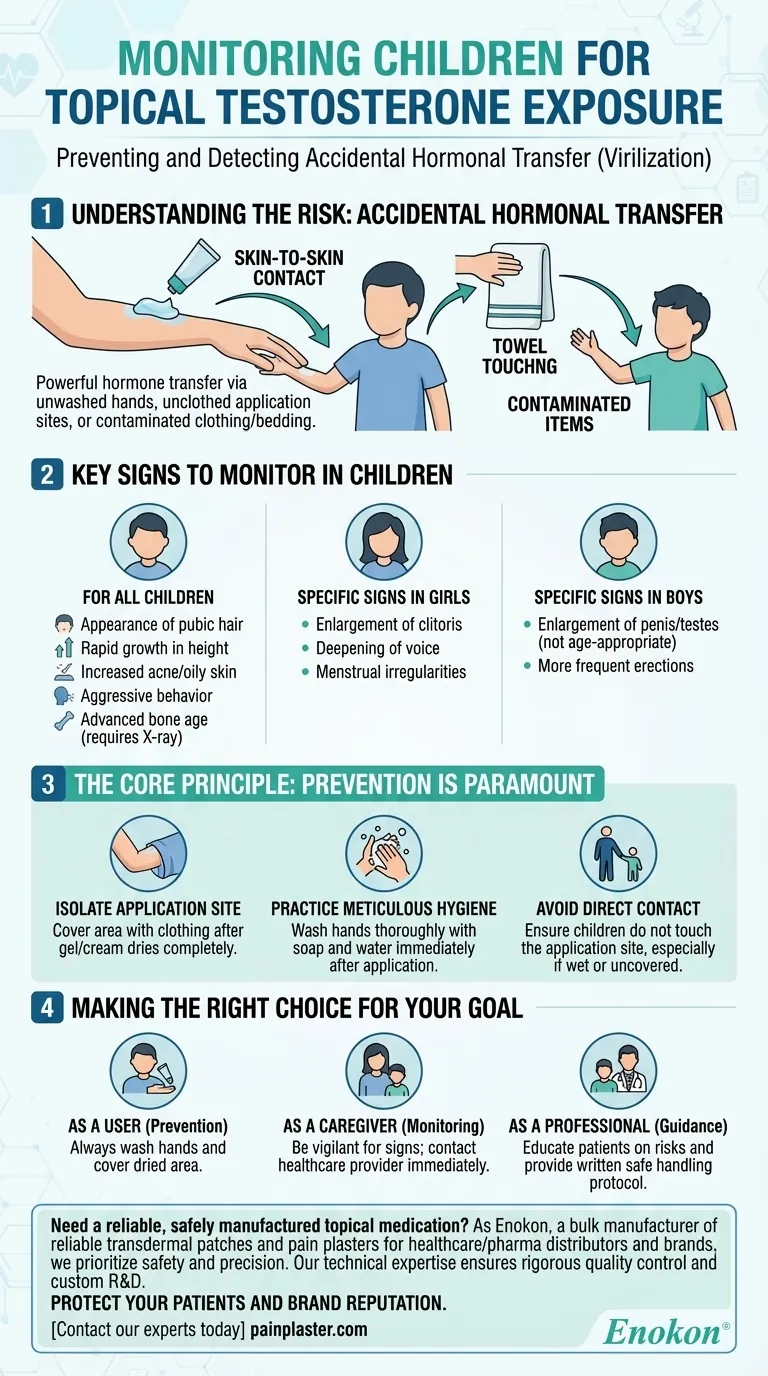
Understanding the Risk: Accidental Hormonal Transfer
How Exposure Happens
Testosterone gels, creams, and liquids can easily transfer from one person to another through direct contact.
The highest risk occurs when a child touches the unwashed or unclothed area of skin where the medication was applied. This can happen through hugging, sleeping in the same bed, or contact with contaminated clothing or towels.
Who Is Most Vulnerable
While any person can be affected, children and women are at the highest risk for significant side effects from accidental exposure due to their lower natural testosterone levels.
A small amount of testosterone transfer that might be unnoticeable to an adult male can cause significant hormonal changes in a child.
Key Signs to Monitor in Children
The FDA directs caregivers to watch for signs of early or inappropriate puberty. These symptoms are the body's reaction to the presence of external androgens like testosterone.
For All Children
- Appearance of pubic hair.
- Rapid growth in height (an early growth spurt).
- Increased acne or oily skin.
- Aggressive behavior or increased libido.
- Advanced bone age (which a doctor would determine via X-ray).
Specific Signs in Girls
- Enlargement of the clitoris.
- Deepening of the voice.
- Changes or irregularities in the menstrual cycle if it has already begun.
Specific Signs in Boys
- Enlargement of the penis or testes that is not age-appropriate.
- More frequent erections.
The Core Principle: Prevention is Paramount
Monitoring is a secondary defense. The primary strategy must always be preventing the drug transfer.
Isolate the Application Site
The person using the testosterone must cover the application area with clothing, such as a t-shirt, after the gel or cream has dried completely.
This creates a physical barrier that minimizes the chance of skin-to-skin transfer.
Practice Meticulous Hygiene
Immediately after applying the medication, the user must wash their hands thoroughly with soap and water.
This simple step prevents the transfer of the hormone from their hands to other people or surfaces.
Avoid Direct Contact
Ensure that children do not have direct skin contact with the application site, especially if it is still wet or has not been covered with clothing.
Making the Right Choice for Your Goal
- If your primary focus is prevention as the user: Always wash your hands immediately after application and cover the treated area with clothing once it has dried. This is the most effective way to protect others.
- If your primary focus is monitoring as a caregiver: Be vigilant for the specific physical and behavioral signs of early puberty and contact a healthcare provider immediately if you notice any changes.
- If your primary focus is clinical guidance as a healthcare professional: Explicitly educate your patient on the risks of secondary exposure and provide them with a clear, written protocol for safe handling to protect their family members.
Proactive prevention and vigilant monitoring are essential to ensure the safety of children in any household where topical testosterone is used.
Summary Table:
| Category | Key Signs & Symptoms to Monitor |
|---|---|
| For All Children | Appearance of pubic hair, rapid growth spurt, increased acne/oily skin, aggressive behavior. |
| Specific to Girls | Enlargement of the clitoris, deepening of the voice, menstrual irregularities. |
| Specific to Boys | Enlargement of the penis/testes (not age-appropriate), more frequent erections. |
Need a reliable, safely manufactured topical medication? As Enokon, a bulk manufacturer of reliable transdermal patches and pain plasters for healthcare/pharma distributors and brands, we prioritize safety and precision in every product. Our technical expertise ensures rigorous quality control and custom R&D for formulations that meet the highest standards. Protect your patients and your brand reputation. Contact our experts today to discuss your development needs.
Visual Guide
Related Products
- Far Infrared Heat Pain Relief Patches Transdermal Patches
- Heating Pain Relief Patches for Menstrual Cramps
- Capsaicin Chili Medicated Pain Relief Patches
- Prostate Pain Kidney Health Care Patch for Men
- Far Infrared Pain Patch Relief Pain Reliever for Back
People Also Ask
- How do Deep Heat Pain Relief Patches provide pain relief? Discover the Drug-Free Mechanism
- How does the Deep Heat Back Patch work? A Drug-Free Solution for Targeted Pain Relief
- Can heat patches be used for fresh injuries? Avoid This Common Mistake for Faster Recovery
- What are the common side effects of using the medicated heat patch? Understanding Risks & Safe Use
- What types of pain can the Deep Heat Pain Relief Back Patch be used for? Targeted Relief for Muscles & Joints












