Non-ionic surfactants are the preferred choice in transdermal formulation because they offer a superior balance between biological safety and functional efficacy. Their uncharged chemical structure significantly minimizes skin irritation compared to ionic alternatives, while their ability to disrupt the stratum corneum ensures deep and effective drug penetration.
Core Takeaway Non-ionic surfactants derive their safety from uncharged polar head groups that minimize toxicity, while achieving efficacy by fluidizing skin lipids and emulsifying sebum. They act as dual-purpose agents: stabilizing the formulation physically while chemically altering the skin barrier to enhance drug diffusion.
The Safety Advantage
The primary reason formulators select non-ionic surfactants over ionic options is the biological tolerance of the skin.
Reduced Irritation Potential
The safety profile of these surfactants is dictated by their head groups. Because they possess uncharged polar head groups, they interact less aggressively with skin proteins than charged (ionic) surfactants. This results in significantly lower irritation and better overall skin tolerance, making them suitable for long-term transdermal applications.
Chemical and Economic Stability
Beyond biological safety, non-ionic surfactants offer formulation stability. Compared to biological lipids like phospholipids, these surfactants are chemically more stable and cost-effective. This makes them a robust structural foundation for drug delivery systems, such as vesicle bilayers, without the high degradation risks associated with natural lipids.
Mechanisms of Efficiency
Efficiency in transdermal delivery is defined by how well a substance helps a drug cross the skin barrier. Non-ionic surfactants achieve this through three specific mechanisms.
Increasing Lipid Fluidity
These surfactants actively penetrate the intercellular regions of the stratum corneum. Once inside, they increase the fluidity of the lipid bilayers. By making the skin's lipid structure more fluid, they reduce the resistance the barrier presents to the drug, thereby improving the drug's diffusion coefficient.
Lipid Extraction and Emulsification
Non-ionic surfactants can mimic the skin's natural lipid environment. This allows them to dissolve and extract lipid components from the stratum corneum. Furthermore, they emulsify sebum, which enhances the thermodynamic coefficient of the drug formulation, allowing for more effective penetration into the cells.
Steric Stabilization
In advanced formulations like nanoparticles, surfactants such as Tween-80 reduce interfacial tension. This provides steric stabilization, which prevents particles from aggregating. The result is a formulation with a narrower particle size distribution and better dispersion, ensuring consistent drug delivery.
Formulation Versatility
Non-ionic surfactants are not limited to acting as mere permeation enhancers; they are functional structural components.
Dual Drug Encapsulation
These surfactants serve as the structural basis for vesicles. Their unique structure allows for the encapsulation of both hydrophilic (water-loving) and hydrophobic (fat-loving) drugs. This versatility allows formulators to deliver a wide range of active pharmaceutical ingredients using a single platform.
Improving Physical Characteristics
Specific surfactants, such as Polysorbate 80, act as solubilizers that improve the physical appearance of the product. They enhance film transparency and physical stability while reducing the greasiness often caused by high concentrations of oily components in patches or gels.
Understanding the Trade-offs
While safe and efficient, the use of non-ionic surfactants requires precise control to avoid formulation failure.
The Critical Role of HLB
The efficacy of these surfactants acts on a spectrum defined by the Hydrophilic-Lipophilic Balance (HLB). There is no "one size fits all" surfactant; the specific HLB value determines the size of delivery vesicles and the efficiency of drug entrapment. Selecting the wrong HLB can lead to unstable formulations or poor drug loading.
Barrier Manipulation Risks
While less irritating than ionic options, the mechanism of "lipid extraction" inherently involves altering the skin barrier. Formulators must balance the concentration of the surfactant to maximize drug flux without compromising the skin's protective function to the point of damage.
Making the Right Choice for Your Goal
When selecting a non-ionic surfactant for your transdermal project, consider your primary objective:
- If your primary focus is Safety and Tolerance: Prioritize surfactants with uncharged polar heads to minimize irritation, specifically avoiding ionic alternatives that disrupt skin proteins.
- If your primary focus is Poorly Soluble Drugs: Utilize surfactants like Polysorbate 80 to act as a solubilizer, improving the partition characteristics and increasing the drug's solubility within the matrix.
- If your primary focus is Controlled Delivery (Vesicles): Select surfactants based on strict HLB calculations to regulate vesicle size and maximize entrapment efficiency.
Ultimately, the optimal surfactant acts as a bridge, stabilizing the drug within the formulation while temporarily unlocking the skin barrier to allow passage.
Summary Table:
| Feature | Key Benefit | Mechanism for Efficiency |
|---|---|---|
| Biological Safety | Minimal Skin Irritation | Uncharged polar head groups reduce protein interaction. |
| Lipid Fluidity | Higher Diffusion Rates | Fluidizes the stratum corneum for easier drug passage. |
| Formulation Stability | Cost-Effective & Durable | Resists chemical degradation compared to natural lipids. |
| Steric Stabilization | Uniform Drug Dispersion | Reduces interfacial tension to prevent particle aggregation. |
| Drug Versatility | Dual Encapsulation | Supports both hydrophilic and hydrophobic active ingredients. |
Partner with Enokon for Expert Transdermal Solutions
Are you looking to enhance your product's efficacy with safe and stable formulations? Enokon is a trusted brand and manufacturer offering professional wholesale transdermal patches and custom R&D solutions.
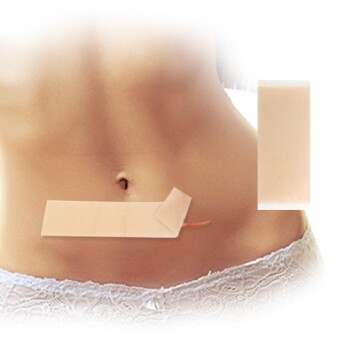
We provide a comprehensive range of transdermal drug delivery products (excluding microneedle technology), including:
- Advanced Pain Relief: Lidocaine, Menthol, Capsicum, Herbal, and Far Infrared patches.
- Specialty Care: Eye Protection, Detox, and Medical Cooling Gel patches.
Our team specializes in balancing safety and performance to bring your vision to market. Contact us today to discuss your custom project and see how our manufacturing expertise can provide the competitive edge your brand needs!
References
- Mohd Yasir, Kashish Bhatia. Status of surfactants as penetration enhancers in transdermal drug delivery. DOI: 10.4103/0975-7406.92724
This article is also based on technical information from Enokon Knowledge Base .
Related Products
- Lidocaine Hydrogel Pain Relief Patch for Pain Relief
- Menthol Gel Pain Relief Patch
- Asthma Cough and Pain Relief Patch for Adults and Kids
- Icy Hot Menthol Medicine Pain Relief Patch
- Far Infrared Heat Pain Relief Patches Transdermal Patches
People Also Ask
- What serious side effects can occur with lidocaine patches? Risks & Safety Tips
- What precautions should be taken when disposing of lidocaine patches? Protect Your Household from Accidental Poisoning
- How should lidocaine patches be applied for optimal use? Maximize Pain Relief with Proper Application
- What are common side effects of lidocaine patches? Key Risks & Safety Tips
- What does research say about the effectiveness of lidocaine patches for chronic low back pain?