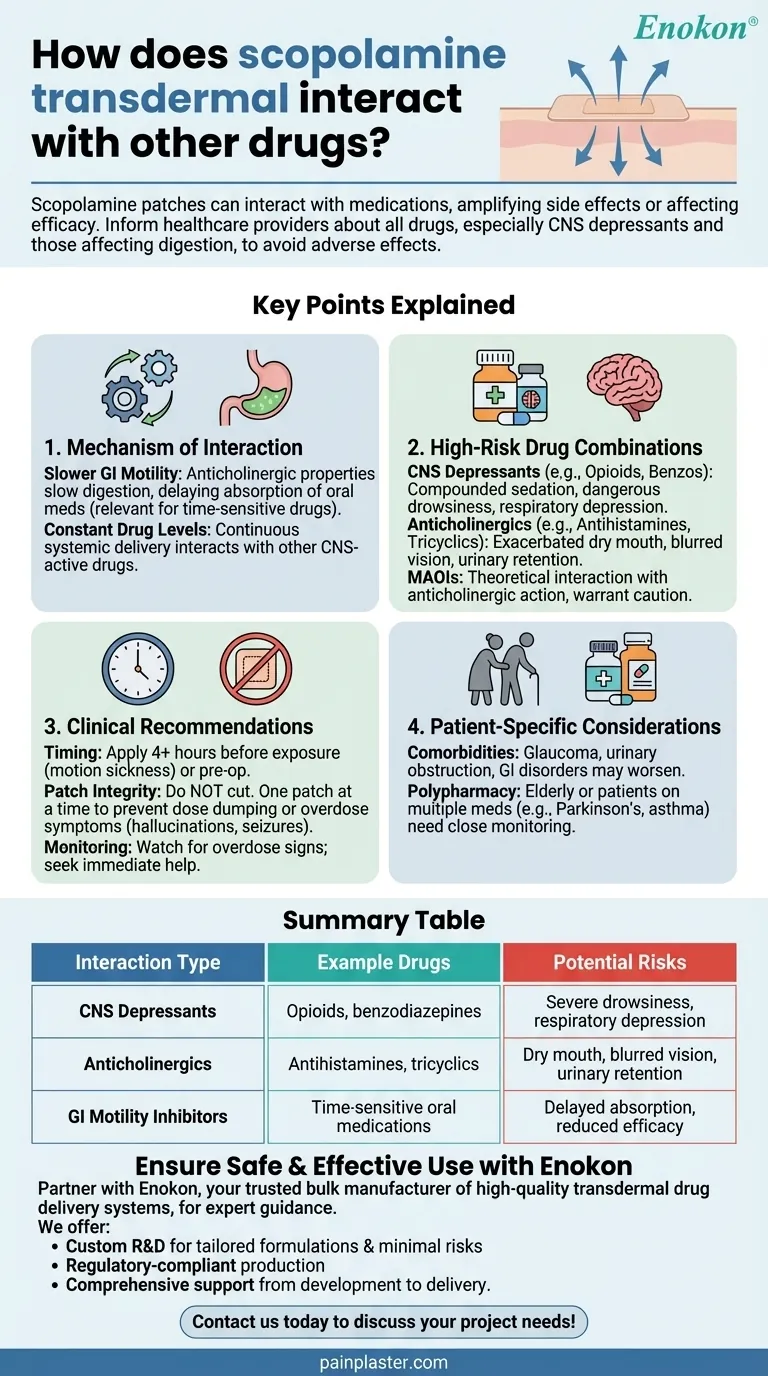
Scopolamine transdermal patches, commonly used for motion sickness and post-operative nausea, can interact with various medications in ways that may amplify side effects or reduce drug efficacy. Key interactions include slowed digestive absorption, additive sedative effects with CNS depressants, and potential complications with anticholinergic drugs. Patients must inform healthcare providers about all medications, especially those affecting the nervous system or digestion, to avoid adverse effects like severe drowsiness, confusion, or urinary retention. Proper application timing (e.g., 4 hours before motion exposure) and avoiding patch alterations are also critical for safety.

Key Points Explained:
-
Mechanism of Interaction
- Scopolamine's anticholinergic properties slow gastrointestinal motility, potentially delaying or reducing absorption of other oral medications. This is particularly relevant for time-sensitive drugs or those with narrow therapeutic windows.
- The Scopolamine Transdermal Patch delivers the drug continuously through the skin, maintaining systemic levels that can interact with other CNS-active drugs.
-
High-Risk Drug Combinations
- CNS Depressants: Opioids, benzodiazepines, and sleep aids can compound scopolamine’s sedative effects, leading to dangerous drowsiness or respiratory depression.
- Anticholinergics: Concurrent use with drugs like antihistamines or tricyclic antidepressants may exacerbate dry mouth, blurred vision, or urinary retention.
- Monoamine Oxidase Inhibitors (MAOIs): Though not directly cited, scopolamine’s anticholinergic action could theoretically interact with MAOIs, warranting caution.
-
Clinical Recommendations
- Timing: For motion sickness, apply the patch at least 4 hours before exposure to allow steady drug levels. Post-surgical use requires pre-operative application.
- Patch Integrity: Cutting the patch can cause dose dumping, leading to toxicity. One patch at a time is essential to avoid overdose symptoms like hallucinations or seizures.
- Monitoring: Watch for signs of overdose (e.g., agitation, rapid heartbeat) and seek immediate medical help if they occur.
-
Patient-Specific Considerations
- Comorbidities: Those with glaucoma, urinary obstruction, or gastrointestinal disorders may experience worsened symptoms due to scopolamine’s effects.
- Polypharmacy: Elderly patients or those on multiple medications (e.g., Parkinson’s drugs, asthma medications) require closer monitoring for additive side effects.
-
Practical Implications for Purchasers
- Education: Ensure patients understand interaction risks and proper usage. For example, pairing scopolamine with over-the-counter cold remedies could be hazardous.
- Inventory Management: Stock alternatives like non-sedating antiemetics for patients on contraindicated drugs.
By addressing these interactions proactively, healthcare providers can mitigate risks while leveraging scopolamine’s benefits—a reminder of how nuanced drug delivery systems shape therapeutic outcomes.
Summary Table:
| Interaction Type | Example Drugs | Potential Risks |
|---|---|---|
| CNS Depressants | Opioids, benzodiazepines | Severe drowsiness, respiratory depression |
| Anticholinergics | Antihistamines, tricyclics | Dry mouth, blurred vision, urinary retention |
| GI Motility Inhibitors | Time-sensitive oral medications | Delayed absorption, reduced efficacy |
Ensure safe and effective use of transdermal patches with expert guidance from Enokon—your trusted bulk manufacturer of high-quality transdermal drug delivery systems. Whether you're a healthcare distributor or pharmaceutical brand, our team provides:
- Custom R&D for tailored formulations to minimize interaction risks
- Regulatory-compliant production of pain plasters and antiemetic patches
- Comprehensive support from development to delivery
Contact us today to discuss your project needs and mitigate drug interaction challenges!
Visual Guide
Related Products
- Far Infrared Heat Pain Relief Patches Transdermal Patches
- Heating Pain Relief Patches for Menstrual Cramps
- Herbal Eye Protection Patch Eye Patch
- Far Infrared Deep Heat Relief Patches Medicated Pain Relief Patches
- Capsaicin Chili Medicated Pain Relief Patches
People Also Ask
- What types of pain can the Deep Heat Pain Relief Back Patch be used for? Targeted Relief for Muscles & Joints
- What did the UK Million Women Study find regarding transdermal versus oral hormone therapy? A Safer Choice for Gallbladder Health
- How quickly does the Deep Heat Pain Relief Back Patch activate and how long does it provide warmth? Get 16-Hour Relief
- What are the common side effects of using the medicated heat patch? Understanding Risks & Safe Use
- Are heat patches safe for all body parts? Key Safety Zones and No-Go Areas Explained













