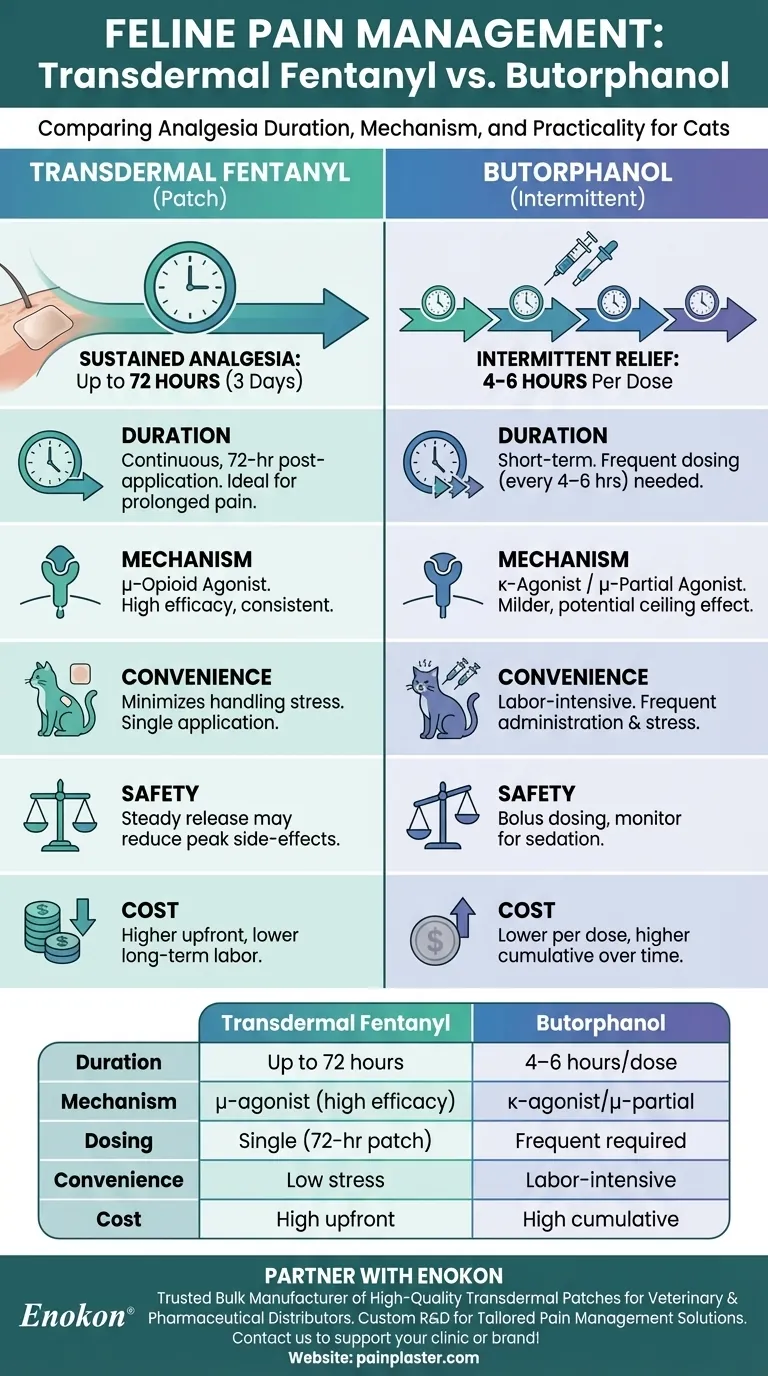
Transdermal fentanyl and butorphanol are both used for pain management in cats, but they differ significantly in duration and mechanism of action. Transdermal fentanyl, delivered via a Fentanyl Transdermal Patch, provides sustained analgesia for up to 72 hours, making it suitable for prolonged pain relief. Butorphanol, typically administered intermittently, offers shorter-term relief and requires more frequent dosing. While both drugs can achieve equivalent analgesia initially, fentanyl's extended duration reduces the need for repeated interventions, enhancing patient comfort and simplifying pain management protocols.

Key Points Explained:
-
Duration of Analgesia
- Transdermal Fentanyl: Delivers continuous pain relief for 72 hours post-application, ideal for post-surgical or chronic pain.
- Butorphanol: Requires intermittent dosing (every 4–6 hours) due to its shorter half-life, making it less practical for long-term use.
-
Mechanism of Action
- Fentanyl: A potent μ-opioid agonist providing consistent, high-efficacy analgesia.
- Butorphanol: A κ-opioid agonist/μ-opioid partial agonist, offering milder analgesia with potential ceiling effects.
-
Clinical Convenience
- The Fentanyl Transdermal Patch minimizes handling stress and dosing errors, while butorphanol demands frequent administration, increasing workload and stress for both cat and caregiver.
-
Safety Considerations
- Both drugs require monitoring for sedation or respiratory depression, but fentanyl’s steady release may reduce peak-side-effect risks compared to butorphanol’s bolus dosing.
-
Cost and Accessibility
- Transdermal fentanyl patches are typically more expensive upfront but may offset costs by reducing labor-intensive dosing. Butorphanol is cheaper per dose but may incur higher cumulative costs over time.
For feline patients needing prolonged analgesia, transdermal fentanyl’s 72-hour efficacy offers a clear advantage, though butorphanol remains useful for acute, short-term pain. Always tailor the choice to the patient’s needs and caregiver capacity.
Summary Table:
| Feature | Transdermal Fentanyl | Butorphanol |
|---|---|---|
| Duration of Analgesia | Up to 72 hours | 4–6 hours per dose |
| Mechanism of Action | μ-opioid agonist (high efficacy) | κ-opioid agonist/μ-opioid partial agonist |
| Dosing Frequency | Single application (72-hour patch) | Frequent dosing required |
| Clinical Convenience | Minimizes handling stress | Labor-intensive |
| Cost Considerations | Higher upfront cost, lower long-term labor costs | Lower per dose, higher cumulative cost |
Need reliable, long-lasting pain relief for feline patients? Partner with Enokon, a trusted bulk manufacturer of high-quality transdermal patches and pain plasters for veterinary and pharmaceutical distributors. Our expertise in custom R&D ensures tailored solutions for your pain management needs. Contact us today to discuss how we can support your clinic or brand with advanced analgesic solutions!
Visual Guide
Related Products
- Far Infrared Deep Heat Relief Patches Medicated Pain Relief Patches
- Menthol Gel Pain Relief Patch
- Icy Hot Menthol Medicine Pain Relief Patch
- Heating Pain Relief Patches for Menstrual Cramps
- Far Infrared Heat Pain Relief Patches Transdermal Patches
People Also Ask
- What are the possible serious side effects of granisetron transdermal patches? Recognize Emergency Signs
- How should transdermal medications be applied to pets? A Vet-Approved Guide
- What are the serious side effects associated with transdermal patches for schizophrenia? Risks from NMS to Skin Reactions
- What are the disadvantages of the contraceptive patch? Weighing Convenience Against Health Risks
- How do statistical analysis and mathematical modeling assist in transdermal drug optimization? Data-Driven Solutions
- What are the modern enhancement methods for transdermal drug delivery? Breakthroughs in Skin Permeation Technology
- How does the contraceptive patch compare in efficacy to oral contraceptives? Convenience vs. Estrogen Exposure
- What are potential side effects of clonidine transdermal? Managing Skin Reactions & Systemic Risks















